When a teenager is struggling with depression, the decision to start an antidepressant isn’t just medical-it’s emotional, scary, and layered with doubt. Parents ask: Is this going to make things worse? Doctors worry: Are we risking suicide? The answer isn’t simple. In 2004, the FDA put a black box warning on all antidepressants for kids and teens, the strongest safety alert they have. It said: These meds may increase suicidal thoughts in young people. That warning is still there today. But what no one talks about enough is what happened after it was issued-fewer teens got treated, and suicide rates went up.
What the Black Box Warning Actually Says
The FDA’s black box warning, updated in 2007 to include young adults up to age 24, doesn’t say antidepressants cause suicide. It says they may increase the risk of suicidal thinking and behavior-especially in the first few weeks of treatment or after a dose change. This isn’t theoretical. In clinical trials with over 4,400 children and teens, about 4% of those on antidepressants showed signs of suicidal thoughts or behaviors. That’s twice the rate seen in kids taking a placebo (2%). No one died in those trials. But even thinking about suicide is serious.
The warning applies to every antidepressant used in teens: fluoxetine (Prozac), sertraline (Zoloft), citalopram (Celexa), venlafaxine (Effexor), bupropion (Wellbutrin), mirtazapine (Remeron)-even the ones doctors usually recommend first. It’s not just about one drug. It’s about all of them. That’s why the FDA requires every prescription bottle to come with a Patient Medication Guide. It’s not a footnote. It’s a legal requirement.
The Unintended Consequences
Here’s the part most people don’t know: after the warning came out, doctors started prescribing antidepressants to teens far less often. A 2023 study in Health Affairs looked at 11 high-quality studies and found a 22.3% drop in antidepressant prescriptions for teens between 2004 and 2006. Visits for depression dropped by 14.5%. Therapy visits fell too. And guess what happened? Suicide attempts-measured by drug poisonings-rose by 21.7%. Completed suicides went up 17.8% in the same period.
This isn’t coincidence. When teens don’t get treatment, their depression gets worse. And untreated depression is the biggest risk factor for suicide. The warning was meant to protect kids. But it may have scared families and doctors away from the very treatment that could save lives. One study found that 76% of child psychiatrists said parents delayed or refused medication because of the warning-adding an average of 3.2 extra weeks before starting treatment. That’s 22 extra days of suffering.
Is the Risk Real-or Overstated?
Not all experts agree the black box warning is helping. Some say the original data was flawed. The clinical trials that led to the warning were short-only up to four months. They didn’t reflect real-world use. Many kids stayed on meds for years. And in those longer-term studies, the risk of suicide didn’t go up-it went down.
A 2023 Cochrane review of 34 trials involving nearly 7,000 teens concluded the evidence on suicidality risk was “low to very low” because the events were so rare and studies were poorly designed. Meanwhile, data from Mayo Clinic showed that among 1,200 teens on SSRIs, 87% improved without any suicidal thoughts. Only 3% had temporary suicidal ideas that went away after adjusting the dose.
And here’s something else: antidepressants work. For teens with moderate to severe depression, they reduce symptoms more than placebo. They help with sleep, energy, concentration, and hope. Without them, many teens can’t go to school, can’t talk to friends, can’t get out of bed. The risk of suicide from depression itself is far higher than the risk from medication.

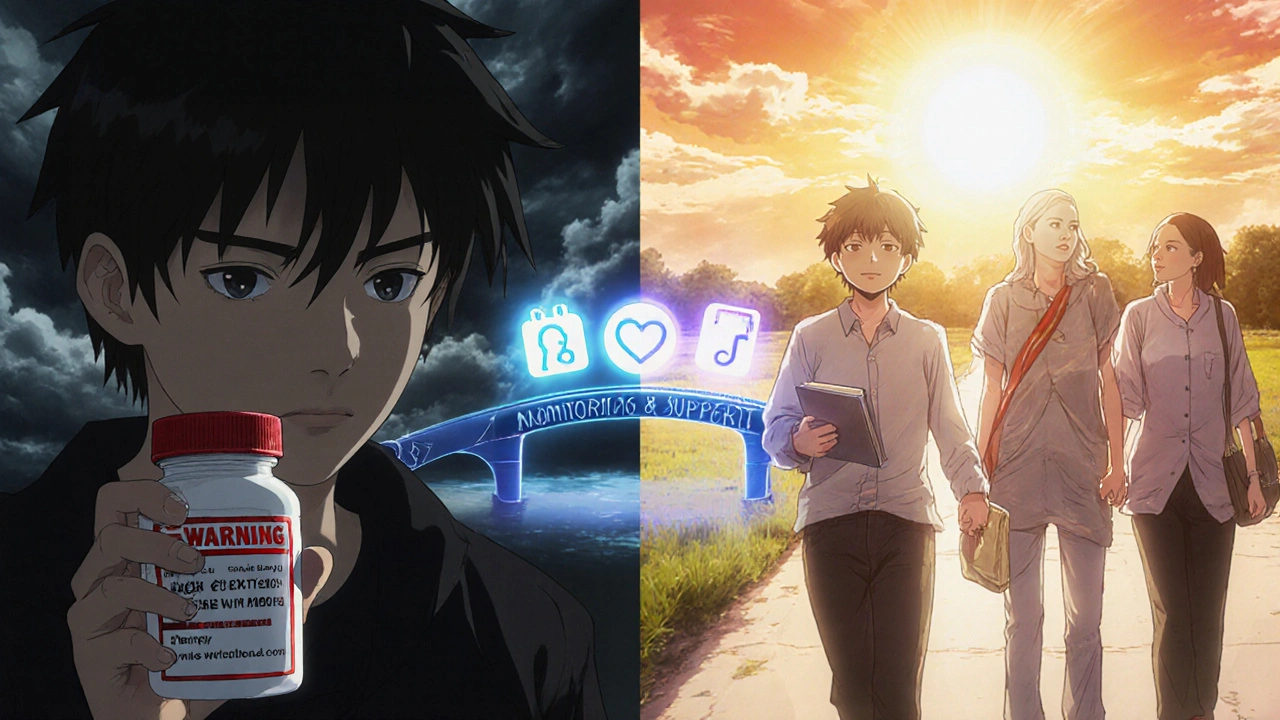
How to Monitor Safely
If you decide to start an antidepressant, the black box warning isn’t a reason to avoid it-it’s a reason to do it right. Monitoring isn’t optional. It’s essential.
- First month: Weekly check-ins with the doctor-either in person or by video. No skipping. This is when risk is highest.
- Second month: Every two weeks. Keep watching for changes: increased agitation, insomnia, irritability, withdrawal, or talk of hopelessness.
- After that: Monthly visits, but stay alert for the first 3-6 months.
Doctors use a tool called the Columbia-Suicide Severity Rating Scale (C-SSRS) at each visit. It’s not a quiz. It’s a conversation. Questions like: “Have you had thoughts about not wanting to live?” “Do you have a plan?” “Have you ever acted on those thoughts?”
Parents need to be involved. Call the clinic if your teen:
- Suddenly becomes more anxious or agitated
- Starts talking about death or dying
- Withdraws from family and friends
- Has trouble sleeping or starts sleeping too much
- Shows a sudden change in grades or behavior
Don’t wait for the next appointment. Call immediately if you’re worried. And remember: this isn’t a sign you’re doing something wrong. It’s a sign you’re paying attention.
What About Therapy?
Antidepressants aren’t the only tool. Therapy-especially cognitive behavioral therapy (CBT)-is just as important. In fact, research shows the best results come when meds and therapy are used together. CBT helps teens challenge negative thoughts, build coping skills, and reconnect with life. For mild depression, therapy alone might be enough. For moderate to severe, combining both gives the best shot at recovery.
But therapy takes time. It’s not always easy to find a good therapist. And insurance doesn’t always cover it. That’s why some families feel stuck-no meds, no therapy, no help. That’s the real crisis.
The Bigger Picture
The black box warning was meant to protect. But it’s now part of a larger problem: we’re failing teens by making treatment harder, not easier. Mental health needs are rising. More teens than ever are reporting depression. Yet prescriptions are still 18.7% below pre-2004 levels. That’s 3.2 million teens a year who might benefit from treatment but aren’t getting it.
Organizations like the American Psychiatric Association and the American Academy of Child and Adolescent Psychiatry are now asking the FDA to revise the warning. They say the benefits outweigh the risks for most teens with moderate to severe depression. A review by the FDA’s advisory committee is scheduled for late 2024. Maybe the warning will change. Maybe it won’t.
But here’s what you can do right now: don’t let fear stop treatment. Talk to your doctor. Ask about therapy. Ask about monitoring. Ask about the data. Ask about alternatives. And if your teen is in crisis, don’t wait. Call 988, the Suicide & Crisis Lifeline. Go to the ER. Get help now.
What’s Next?
Antidepressants aren’t magic pills. They’re tools. And like any tool, they work best when used carefully. The black box warning isn’t a reason to avoid them-it’s a reason to use them wisely. With proper monitoring, the risk is small. The reward-returning a teen to life-is huge.
If you’re a parent, don’t be afraid to ask questions. If you’re a teen, don’t be afraid to speak up. Depression lies. It tells you you’re alone. But you’re not. Help is out there. And it works.
Do antidepressants cause suicide in teens?
No, antidepressants don’t cause suicide. But in the first few weeks of treatment, they may increase the risk of suicidal thoughts or behaviors in some teens. This is rare-about 4% in clinical trials versus 2% on placebo-and no suicides occurred in those studies. The bigger risk is untreated depression, which is the leading cause of teen suicide.
Which antidepressants are safest for teens?
Fluoxetine (Prozac) is the only antidepressant FDA-approved specifically for teens with depression. Sertraline (Zoloft) and escitalopram (Lexapro) are also commonly used and have strong evidence for safety and effectiveness in adolescents. All antidepressants carry the same black box warning, but fluoxetine has the most data supporting its use in this age group.
How long should a teen stay on antidepressants?
Most doctors recommend staying on antidepressants for at least 6 to 12 months after symptoms improve. Stopping too soon increases the risk of relapse. For teens with recurrent depression, longer-term use-even years-may be necessary. Never stop suddenly. Tapering under a doctor’s guidance is critical.
Can therapy replace antidepressants for teens?
For mild depression, therapy alone-especially cognitive behavioral therapy (CBT)-can be very effective. For moderate to severe depression, combining therapy with medication gives the best results. Therapy helps build skills, but medication can help restore the brain’s ability to respond to those skills. They’re not alternatives-they’re partners.
What should I do if my teen has suicidal thoughts after starting medication?
Call your doctor immediately. Don’t wait for the next appointment. If the thoughts are intense or your teen has a plan, go to the nearest emergency room or call 988. This doesn’t mean the medication failed-it means close monitoring is working. Many teens experience temporary increases in suicidal thoughts that resolve with a dose adjustment or added support. The key is acting fast.
Final Thoughts
The black box warning is real. But so is the suffering of teens who don’t get help. The answer isn’t to avoid antidepressants-it’s to use them with care, with support, and with eyes wide open. Treatment saves lives. Fear shouldn’t stop it.


Bartholemy Tuite
November 24, 2025 AT 10:18Look i get the warning and all but lets be real here the real problem isnt the meds its the system that makes you wait 6 months for a therapist and then charges you 300 bucks a session
My cousin was on zoloft for a year after a bad breakup and yeah he had some jittery weeks but he also went from not leaving his room to getting a part time job and starting to play guitar again
Thats not magic thats medicine working
Meanwhile the kid down the street who got told to just meditate and drink chamomile tea ended up in the ER last winter
Its not about fear its about access and we keep pretending this is just a medical issue when its a social disaster
Doctors arent the villains here the insurance companies are
And the FDA warning while well intentioned became a legal shield for inaction
Im not saying its risk free but its less risky than doing nothing
Also why are we still having this conversation in 2025 when we have apps that track mood and AI chatbots that can do CBT for 5 bucks a month
We need to stop treating mental health like its a luxury and start treating it like a basic human right
Neoma Geoghegan
November 24, 2025 AT 23:50Black box warning = red flag for parents = delay = worse outcomes
Its not the drug its the delay
Nikki C
November 26, 2025 AT 20:14My sister started fluoxetine at 16
First two weeks she cried every night
Then she started laughing again
Not because it was magic
Because the fog lifted
She still sees a therapist twice a month
And yeah we check in every day
But she graduated college last year
And she just got engaged
What would have happened if we listened to the fear instead of the data
Im not saying its perfect
But its better than watching someone disappear
Alex Dubrovin
November 27, 2025 AT 17:18ive been on citalopram for 3 years
never had suicidal thoughts
did have panic attacks before
now i can drive to work without shaking
the warning scared me at first
but my doc watched me like a hawk
and it worked
why are we scared of helping
Jacob McConaghy
November 28, 2025 AT 18:50Here’s the thing nobody wants to say out loud
The black box warning is a political tool disguised as medical advice
It was born from fear not science
And now its being used to justify doing nothing
Im not saying every teen needs meds
But when you have a kid who cant get out of bed for 8 months
And you tell them to wait for therapy that costs 200 an hour
And you tell them the meds might kill them
Youre not protecting them
Youre abandoning them
And then you wonder why suicide rates went up
The real danger is the silence
Not the pill
Vineeta Puri
November 30, 2025 AT 05:18While the intent behind the black box warning is commendable, the unintended consequences have been profoundly detrimental to adolescent mental health outcomes.
Empirical data indicates a statistically significant correlation between reduced pharmacological intervention and increased suicidal behaviors in this demographic.
It is imperative that clinical guidelines prioritize evidence-based practice over precautionary rhetoric that lacks longitudinal validation.
Therapeutic alliance, vigilant monitoring, and integrated care models remain the gold standard.
Delaying treatment due to fear is not ethical-it is negligent.
Let us not mistake caution for compassion.
Victoria Stanley
December 1, 2025 AT 22:26My daughter started sertraline at 15
First week she was tired and weird
Second week she asked to go to the mall
Third week she texted me a meme
That was the moment i knew
It wasn't about the drug
It was about giving her back her life
And yes we had weekly calls with her doctor
But the fear of the warning almost cost us that
Don't let bureaucracy steal your kid's future
Andy Louis-Charles
December 1, 2025 AT 22:37just want to say i love how the article says "call if your teen withdraws"
but nobody talks about how hard it is to notice that
my son stopped talking to me for 3 months
i thought he was just being a teen
turns out he was spiraling
and i had no idea
the warning is good
but we need better education for parents too
like how to spot the quiet signs
not just the loud ones
and maybe a hotline for parents who are scared to ask
🙏Douglas cardoza
December 3, 2025 AT 18:08my therapist said the black box warning is like putting a sign on a fire extinguisher that says "may cause minor burns"
and then people dont use it when the house is on fire
we need to stop treating mental health like its dangerous
its dangerous to do nothing
Akash Chopda
December 4, 2025 AT 00:02the real story is the FDA got pressured by pharma to scare parents so they could sell more therapy apps and insurance loopholes
they knew the numbers were fake
they just needed a scare tactic
now parents are too scared to help
and the kids are dying
and nobody talks about it
because the system is rigged