Blocked-up nose: fast relief and when to get help
A blocked-up nose can wreck sleep, make eating annoying, and leave you foggy-headed. Most congestion comes from colds, allergies, or dry air — and you can ease it with a few simple moves. Below are practical tips that work quickly and safely for most adults and kids.
Fast home fixes
Start with saline nasal spray or rinse. Saline thins mucus and clears nostrils without drugs; use it several times daily. Steam helps too: inhale steam over a bowl or take a hot shower for 5–10 minutes to loosen stuffiness. Stay hydrated — water and warm broths thin secretions. Use a humidifier at night to keep air moist, especially in heated homes. Raise your head while sleeping by adding a pillow; gravity helps drainage.
Over-the-counter options can help when home care isn't enough. Short-term topical decongestant sprays (oxymetazoline) work fast but use no more than three days to avoid rebound congestion. Oral decongestants like pseudoephedrine relieve swollen nasal tissue but can raise blood pressure and cause jitteriness; check with a pharmacist if you have heart problems. Antihistamines help if allergies are the cause — newer non-drowsy options ease runny nose and sneezing. Nasal steroid sprays reduce inflammation and are safe for long-term allergy control, but they take a few days to reach full effect.
Try simple natural aids: warm compresses on the face can ease sinus pressure. Peppermint or menthol rubs under the nose sometimes feel soothing, but avoid applying inside the nose. Avoid smoke, strong perfumes, and other irritants that make congestion worse.
When to see a doctor
Most stuffy noses clear in a week or two. See a doctor sooner if you have high fever, severe facial pain, swelling around the eyes, bloody discharge, or symptoms that last beyond 10 days. Chronic or recurring congestion could mean allergies, nasal polyps, a deviated septum, or less common conditions that need a targeted plan. For children under two, check with a pediatrician before using any decongestant products. If you use nasal steroids or other prescription meds, follow the doctor’s instructions and report side effects like nosebleeds or persistent irritation.
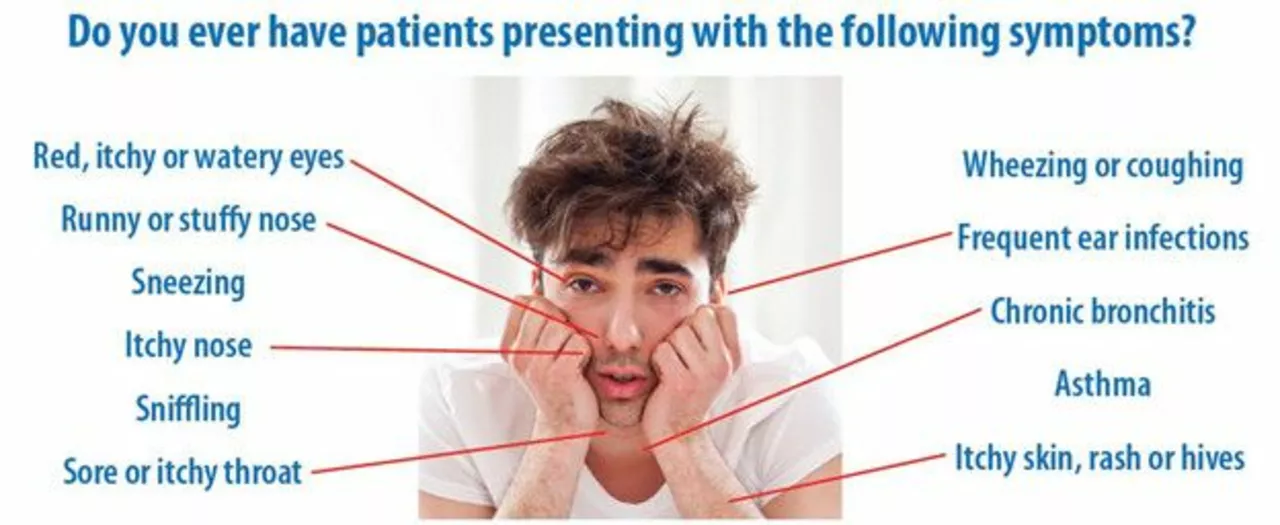
Want targeted help? Our site has guides on allergy medicines like olopatadine, links between asthma and lung issues, and when inhalers or steroid sprays fit into care. That info can help you and your clinician build a plan so stuffy noses stop returning.
Short checklist: saline rinses, steam, humidifier, head elevation, limit topical decongestant use, try antihistamines for allergies, and see a doctor for severe or long-lasting symptoms. Small changes usually bring big relief quickly.
Pregnant people and those with high blood pressure should talk to their doctor before taking oral decongestants. Use sterile or boiled then cooled water for rinses to avoid infections, and clean devices after each use. If you have chronic lung disease like COPD or cystic fibrosis, work with a specialist—stuffy noses can affect breathing and need tailored care. Keeping a symptom diary (triggers, timing, treatments used) helps your clinician pick the right tests and medicines faster. You can get relief.