Neuroleptic Malignant Syndrome (NMS) isn’t something most people hear about until it’s too late. It’s rare-occurring in as few as 1 in 5,000 people taking antipsychotic meds-but when it happens, it’s life-threatening. Imagine your muscles locking up like concrete, your body temperature spiking past 105°F, and your mind slipping into silence. You’re not having a psychotic break. You’re not just sick. You’re experiencing NMS-a medical emergency that can kill if missed.
What Exactly Is Neuroleptic Malignant Syndrome?
NMS is a severe reaction to drugs that block dopamine in the brain. That includes older antipsychotics like haloperidol and chlorpromazine, but also newer ones like risperidone and olanzapine. Even some anti-nausea meds like metoclopramide and promethazine can trigger it. The core problem? Dopamine isn’t just about mood-it controls movement, body temperature, and autonomic functions like heart rate and sweating. When these receptors get blocked too hard or too fast, your body loses control.
The first signs don’t come out of nowhere. They usually show up within the first two weeks of starting or increasing a dose. Sometimes it’s as fast as 48 hours. The classic signs are a four-part pattern: muscle rigidity, high fever, mental confusion, and wild autonomic swings. You might see someone who’s rigid like a statue, sweating buckets one minute and shivering the next, with a pulse racing past 100 beats per minute and blood pressure jumping up and down. Their eyes might be glazed over-or they might be screaming in terror, unable to speak.
How Is NMS Different From Other Conditions?
Doctors often mistake NMS for something else. That’s dangerous. It looks like a worsening psychiatric episode. Or a severe infection. Or even heatstroke. But here’s what sets it apart:
- vs. Serotonin Syndrome: Serotonin syndrome comes on fast-within hours-and features twitching muscles, clonus (involuntary jerking), and diarrhea. NMS moves slower. Its rigidity is uniform and deep-called ‘lead pipe’ rigidity-where you can’t bend someone’s arm no matter how hard you try. No clonus. No GI symptoms.
- vs. Malignant Hyperthermia: Malignant hyperthermia happens during anesthesia, not from psychiatric meds. It’s faster, with jaw muscle spasms and rapid breathing. NMS doesn’t have that.
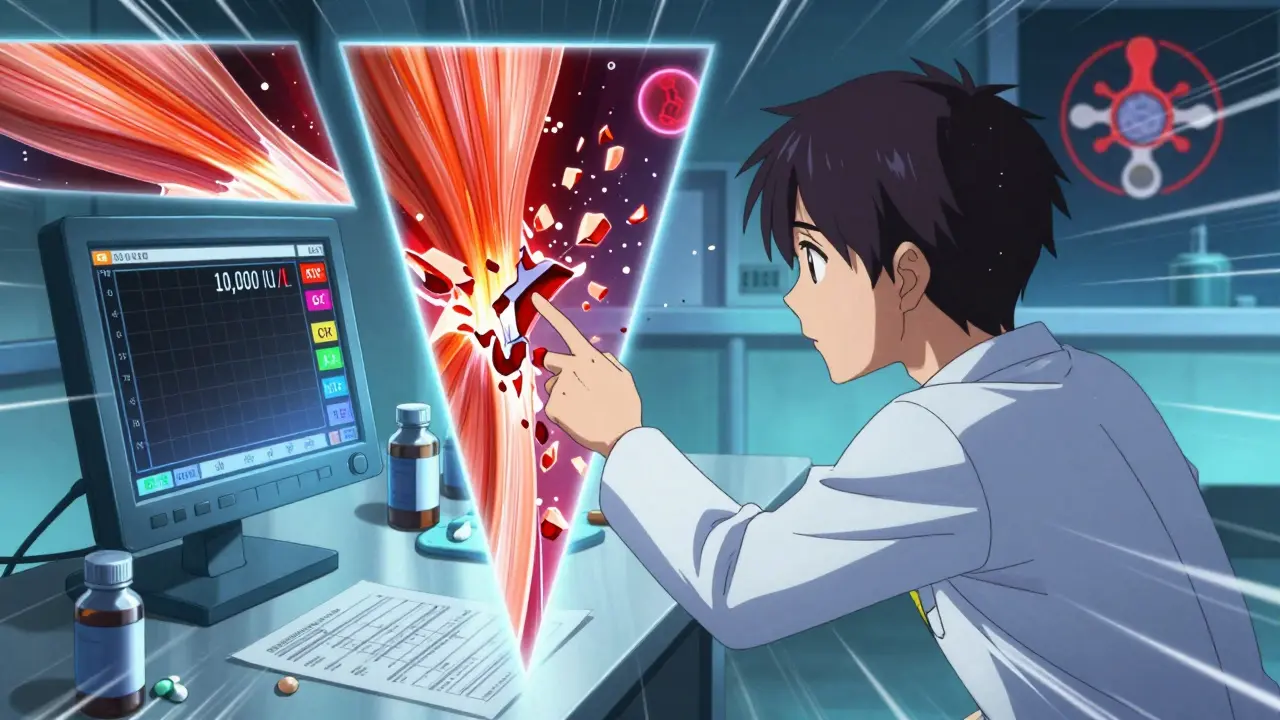
One big clue? Creatine kinase (CK) levels. In NMS, CK skyrockets-often over 1,000 IU/L, sometimes hitting 100,000. That’s because your muscles are breaking down. This isn’t just pain. It’s muscle death. And when that muscle debris floods your kidneys, you risk kidney failure. About 30% of NMS cases lead to acute kidney injury.
Who’s Most at Risk?
NMS doesn’t pick favorites, but certain factors raise the odds:
- Starting or increasing a high-potency antipsychotic like haloperidol by more than 5 mg per day
- Receiving antipsychotics by injection instead of pills
- Being on lithium along with an antipsychotic
- Being young and male (men are twice as likely to develop it)
- Having bipolar disorder rather than schizophrenia
Even more surprising: 10% of cases happen in people who’ve been on the same dose for months or years. No dose change. No new meds. Just… out of nowhere. That’s why doctors can’t rely on ‘risk factors’ alone.
And here’s something few realize: NMS can also happen if you suddenly stop Parkinson’s meds like levodopa. Your body needs dopamine. Take it away too fast? Your brain panics. Symptoms can show up in 24 to 72 hours.
What Happens in the Body?
At its core, NMS is a dopamine crisis. Dopamine receptors in the hypothalamus regulate body temperature. Block those, and your brain can’t cool you down. Dopamine in the basal ganglia controls movement. Block those, and muscles freeze. Dopamine in the brainstem helps manage heart rate, breathing, and blood pressure. Block those, and your autonomic nervous system goes haywire.
That’s why the symptoms hit in a pattern: mental status changes first (confusion, agitation, mutism), then rigidity, then fever, then autonomic chaos. It’s not random. It’s the brain and body screaming because dopamine signaling has collapsed.
Lab tests show more than just high CK. You’ll often see:
- White blood cell count above 12,000/µL
- Low serum iron (under 60 µg/dL)
- Metabolic acidosis (bicarbonate below 22 mEq/L)
- Low oxygen levels
- High potassium
These aren’t random numbers. They’re signs your body is under extreme stress. The liver might get damaged. The kidneys might shut down. Electrolytes go wild. Without intervention, multi-organ failure follows.
How Is It Treated?
Time is everything. The longer you wait, the higher the chance of death. The Cleveland Clinic’s protocol is clear:
- Stop the drug immediately. All antipsychotics. All dopamine blockers. No exceptions.
- Cool the body. If temperature is over 102°F (38.9°C), use cooling blankets, ice packs, and IV fluids. Don’t wait.
- Hydrate aggressively. Give 1-2 liters of IV fluids fast, then maintain 100-150 mL/hour. This protects the kidneys from muscle breakdown products.
- Use dantrolene. This muscle relaxant is the go-to drug. Start with 1-2.5 mg/kg IV, and repeat as needed up to 10 mg/kg. It helps break the muscle rigidity cycle.
- Consider bromocriptine or apomorphine. These restore dopamine activity. Bromocriptine is oral, given every 8 hours. Apomorphine (still experimental) is being tested as a nasal spray-and early results show it can lower fever in 4 hours.
CK levels are tracked every 6 to 12 hours. They usually peak at 72 to 96 hours after onset. If they keep climbing, you’re still in danger. If they drop, you’re turning the corner.
One in four severe cases needs dialysis. That’s how serious the kidney damage can get.

What’s the Survival Rate?
Twenty years ago, NMS killed 20% of those who got it. Today? Around 5%. Why? Because doctors are learning to spot it faster. In 2021, a study showed only 60% of ER doctors correctly diagnosed NMS. That’s improving. AI tools now scan electronic records for early warning signs-like rising CK, fever, and recent antipsychotic use-and flag potential cases before symptoms get severe.
Survivors often face long recoveries. Muscle weakness can last weeks. Some take 8 weeks just to walk again. And here’s the hidden toll: 65% of survivors are terrified to take antipsychotics again-even if they need them. That creates a nightmare for their care teams. How do you treat psychosis without triggering NMS again?
Can It Happen Again?
Yes. But it’s rare. If you’ve had NMS once, your risk of recurrence is low-around 1% to 3%-if you avoid the same drugs. But you can’t just switch to any other antipsychotic. Some carry similar risks. The safest path? Work with a specialist. Start with a low-dose atypical antipsychotic like quetiapine or clozapine, which have lower dopamine-blocking power. Monitor closely. Go slow.
There’s hope on the horizon. Newer drugs are being designed to target psychosis without over-blocking dopamine. In 2023, the FDA required stronger warnings on all antipsychotic labels. The message is clear: NMS can happen even with ‘normal’ doses, even in people with no risk factors.
What Should You Do If You Suspect NMS?
If you or someone you know is on an antipsychotic and suddenly develops:
- Stiff muscles that won’t move
- Fever above 100.4°F
- Confusion, mutism, or agitation
- Rapid heartbeat, sweating, or blood pressure swings
-get to an emergency room immediately. Tell them: ‘I think this might be Neuroleptic Malignant Syndrome.’ Don’t wait for them to figure it out. Say it out loud. It’s rare, but it’s real. And if you’re the one who knows the signs, you might save a life.
Can NMS happen with newer antipsychotics?
Yes. While the risk is much lower with second-generation antipsychotics like risperidone or olanzapine-around 0.01% to 0.02%-it still happens. Most cases today involve these newer drugs because they’re used far more often than older ones like haloperidol. No antipsychotic is completely risk-free.
How long does it take to recover from NMS?
With prompt treatment, most people start improving within 7 to 10 days. But full recovery can take weeks to months. Muscle weakness, fatigue, and cognitive fog are common for weeks after. Some survivors report lingering stiffness or reduced coordination for over a month. The body needs time to heal from severe muscle damage.
Is dantrolene always necessary?
Not always, but it’s strongly recommended. Dantrolene helps reduce muscle rigidity and lowers the risk of rhabdomyolysis and kidney damage. In severe cases, it’s lifesaving. Some doctors use it even if the diagnosis isn’t 100% certain-because the risks of waiting outweigh the risks of giving it.
Can NMS be prevented?
You can reduce the risk. Avoid rapid dose increases, especially with high-potency drugs. Never give antipsychotics by injection unless absolutely necessary. Avoid combining antipsychotics with lithium. Monitor for early signs in the first two weeks. And never ignore unexplained fever or rigidity in someone on these meds.
Can NMS occur without antipsychotics?
Yes. About 15% of cases are triggered by non-antipsychotic dopamine blockers like metoclopramide (for nausea) or promethazine (for allergies). Also, sudden withdrawal of Parkinson’s medications like levodopa can trigger NMS-like symptoms in up to 5% of cases.
Why is CK level so important in diagnosing NMS?
Creatine kinase (CK) measures muscle damage. In NMS, muscles are locked in constant contraction, leading to massive breakdown. CK levels above 1,000 IU/L are common; levels over 10,000 are a red flag. Rising CK confirms rhabdomyolysis and signals kidney risk. Tracking CK helps doctors know if treatment is working and when it’s safe to stop aggressive care.
If you’re on an antipsychotic, don’t panic. NMS is extremely rare. But know the signs. Speak up if something feels wrong. And if you’re a caregiver or family member-remember: muscle stiffness and fever aren’t just ‘bad days.’ They could be the first warning of something far more serious.


Akshaya Gandra _ Student - EastCaryMS
January 3, 2026 AT 19:59wait so even anti-nausea meds can do this?? i had promethazine last month for vomiting and now i’m kinda scared to take anything again lol
Peyton Feuer
January 4, 2026 AT 04:48my aunt had this after a haloperidol shot-doctors thought it was a psychotic break until her muscles locked up and she couldn’t breathe. she’s fine now but takes quetiapine low dose now. never ignore stiffness + fever.
Allen Ye
January 4, 2026 AT 20:18what fascinates me isn’t just the pathophysiology-it’s how we’ve normalized the idea that psychiatric meds are ‘safe’ because they’re ‘modern.’ we forget dopamine isn’t just a mood molecule-it’s the conductor of movement, thermoregulation, autonomic stability. when you blunt it too hard, you don’t just change behavior-you disable a biological orchestra. and the fact that we still rely on muscle rigidity and CK levels as diagnostic anchors in 2024? that’s not science-it’s reactive triage. we need predictive biomarkers, not late-stage symptoms. the real tragedy isn’t NMS-it’s that we treat it like an outlier instead of a systemic blind spot in how we pharmacologically manage the brain.
melissa cucic
January 5, 2026 AT 12:00Thank you for this detailed, clinically accurate overview. It’s alarming how often NMS is misdiagnosed as agitation or delirium, particularly in elderly populations. The ‘lead-pipe’ rigidity is a hallmark that should be taught in every medical orientation-yet it’s rarely emphasized. I hope this reaches not only clinicians but also caregivers who may be the first to notice subtle changes in mobility or temperature. Knowledge is, indeed, the most immediate intervention.
Jay Tejada
January 5, 2026 AT 22:31my brother got NMS from metoclopramide after his chemo. they thought he was just dehydrated. took 3 days to figure it out. he’s okay now but still gets muscle cramps at night. i wish i’d known then what i know now.
Cassie Tynan
January 7, 2026 AT 19:10so let me get this straight-we’re giving people brain-altering drugs like candy, then acting shocked when their bodies revolt? revolutionary.
Aaron Mercado
January 7, 2026 AT 22:38People need to STOP taking antipsychotics like they’re vitamins. I’ve seen too many ‘just one more pill’ stories. This isn’t a side effect-it’s a biological bomb. If you’re on these meds and you feel ‘off,’ don’t ‘wait and see.’ Go to the ER. Say the words. Don’t let pride kill you. I’m not being dramatic-I’ve buried people who didn’t.
John Wilmerding
January 8, 2026 AT 00:07Thank you for sharing this comprehensive overview. As a healthcare provider, I can confirm that early recognition remains the single most critical factor in reducing mortality. I routinely educate patients and families about the ‘4 S’s’: Stiffness, Fever, Stupor, and Sympathetic instability. We also include a printed handout in every new antipsychotic prescription packet. If you are ever in doubt, err on the side of caution-NMS is not a diagnosis you want to make in retrospect.
Siobhan Goggin
January 8, 2026 AT 20:14Thank you for writing this. I’m a nurse who’s seen two cases in 12 years. Both survived because their families insisted on ‘checking for NMS.’ Don’t be afraid to ask. You’re not being difficult-you’re being lifesaving.
mark etang
January 9, 2026 AT 13:54It is imperative that medical professionals recognize that Neuroleptic Malignant Syndrome is not a rare curiosity, but rather a potentially lethal iatrogenic event that demands immediate, protocol-driven intervention. The use of dantrolene, aggressive hydration, and dopamine agonists should be considered standard of care in suspected cases. Furthermore, institutional protocols must be standardized across emergency departments to reduce diagnostic delay. Patient outcomes improve dramatically with rapid, coordinated care.