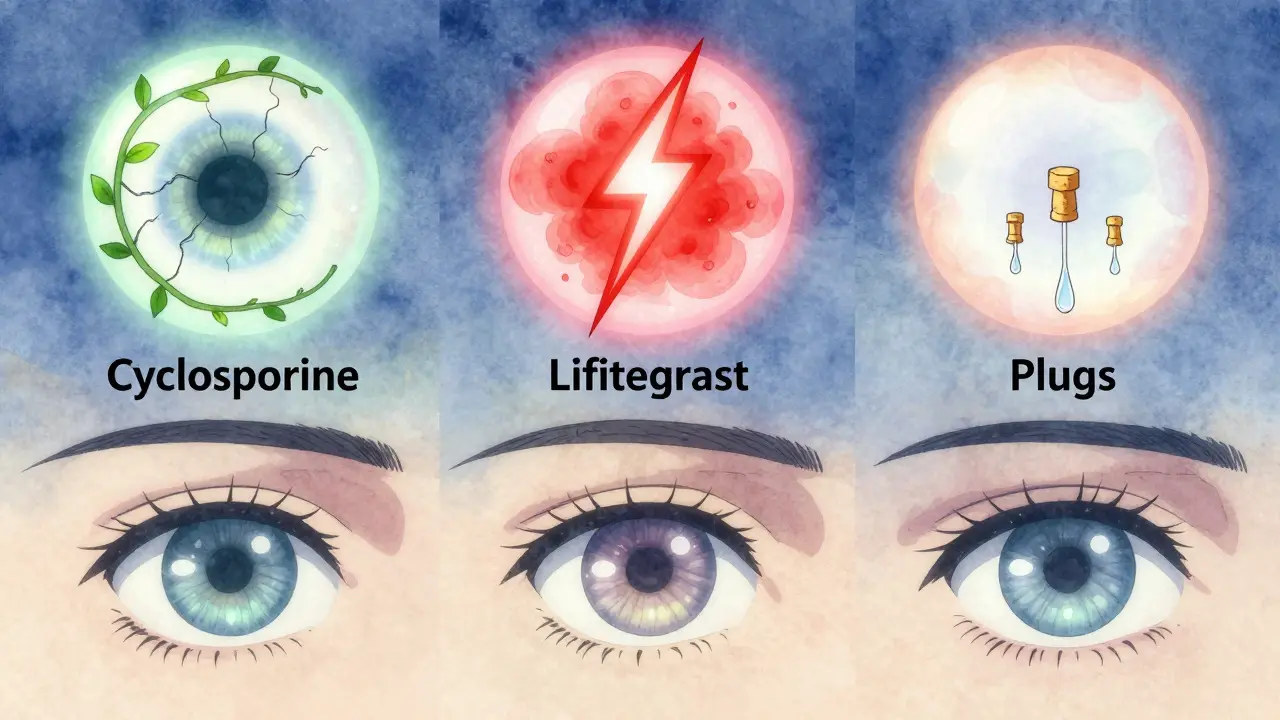
If you’ve been squinting in front of your screen all day, blinking more than usual, or feeling like there’s sand in your eyes - you’re not alone. Over 16 million Americans have been diagnosed with dry eye disease, and that number keeps climbing, especially as we spend more time staring at phones and computers. For many, over-the-counter drops don’t cut it anymore. When that happens, doctors turn to three proven options: cyclosporine, lifitegrast, and punctal plugs. Each works differently, has different timelines, and comes with its own set of pros and cons. Knowing how they compare can save you months of frustration - and money.
How Cyclosporine (Restasis, Cequa) Works
Cyclosporine isn’t a tear replacement. It’s an immune system modulator. Think of it like turning down the volume on inflammation in your eyes. Chronic dry eye isn’t just about not making enough tears - it’s often caused by your body’s own immune system attacking the tear glands. Cyclosporine, sold as Restasis and Cequa, blocks that attack so your eyes can start making tears again - naturally.
The FDA approved Restasis back in 2002, and it’s been the gold standard ever since. You apply it twice a day, about 12 hours apart. It’s not fast. Most people don’t feel better until 3 to 6 months in. That’s hard to stick with, especially when your eyes burn the first few weeks. But here’s the thing: if you stick with it, the results last. A 2023 study in JAMA Ophthalmology showed 71.6% of users had significant improvement in corneal staining - a key sign of eye surface damage - compared to just under 60% on placebo.
Generic versions of the single-use vials are now available, bringing the cost down from $600 to around $300 a month. Restasis MultiDose uses a special gel to help the medicine stick around longer. Cequa, the newer 0.1% version, uses nanomicelles to improve absorption - meaning more of the drug actually reaches your eye. But even with better tech, you still need patience. No shortcuts.
Lifitegrast (Xiidra): Faster Relief, Different Side Effects
If you need relief now, lifitegrast (Xiidra) is your best bet. Approved in 2016, it works differently than cyclosporine. Instead of calming the immune system long-term, it blocks a specific protein (LFA-1) that triggers inflammation and dryness. The result? Faster symptom relief.
In clinical trials, 47% of people using Xiidra saw a noticeable drop in dryness within two weeks. That’s a big deal when you’re struggling to read your phone or drive at night. But it’s not magic. You still need to use it twice daily. And there’s a catch: about 1 in 5 people report a strong metallic or bitter taste. It’s not dangerous, but it’s annoying enough that some stop taking it.
People who’ve tried both say Xiidra feels more like a quick fix. One Reddit user wrote, “I noticed less burning in 10 days - but my eyes still feel tired by 3 p.m.” That’s normal. Xiidra doesn’t rebuild your tear production like cyclosporine does. It just makes the inflammation less angry. So it’s great for flare-ups or if you can’t wait months for results. But if you want long-term healing, you’ll likely need to pair it with something else.
Punctal Plugs: The Mechanical Solution
Punctal plugs are tiny devices inserted into the small openings (puncta) where tears normally drain out of your eyes. Think of them like corks in a sink. By blocking the drain, your natural tears stay on the eye longer. They’ve been around since the 1970s and are still widely used today.
There are two main types: temporary (collagen) and permanent (silicone). Collagen plugs dissolve on their own in 3 to 10 days - perfect for testing if plugs will help. Silicone plugs last years and can be removed if needed. The procedure takes less than 10 minutes and is done right in the doctor’s office. No anesthesia, no downtime.
Patients often feel immediate relief. “I stopped watering constantly after the plugs,” said one user on RealSelf. That’s because dry eye isn’t always about not enough tears - sometimes it’s about tears draining away too fast. But plugs don’t fix the root cause. If your tear quality is poor or inflammation is high, plugs alone won’t help much. Studies show they improve tear volume by about 1.8mm on the Schirmer test, but don’t significantly reduce symptoms like burning or grittiness.
There are downsides. About 23% of temporary plugs fall out within two weeks. Permanent ones can feel uncomfortable or poke the eye. Extrusion (the plug pushing out) happens in nearly 30% of cases, especially if you rub your eyes or wear contacts. Still, for people with moderate to severe dry eye and low tear production, plugs are one of the most predictable tools doctors have.

Comparing the Three: Speed, Cost, and Real-World Results
| Feature | Cyclosporine (Restasis/Cequa) | Lifitegrast (Xiidra) | Punctal Plugs |
|---|---|---|---|
| How it works | Reduces inflammation to boost natural tear production | Blocks inflammatory protein for faster symptom relief | Blocks tear drainage to conserve existing tears |
| Time to feel better | 3-6 months | 1-2 weeks | Immediate |
| Dosing | Twice daily, 12 hours apart | Twice daily | One-time procedure |
| Cost per month | $300-$590 (generic vs. brand) | $620 | $150-$300 per insertion (plus office visit) |
| Common side effects | Burning, stinging (73% in first weeks) | Metallic taste (42%), eye irritation | Discomfort, extrusion (28%), tearing |
| Best for | Chronic, moderate-to-severe dry eye with inflammation | Patients needing quick relief or intolerant to cyclosporine | Low tear production, no inflammation, or as add-on therapy |
| Long-term benefit | Yes - rebuilds tear production | No - symptom control only | Yes - if plug stays in |
Here’s what most patients don’t realize: these aren’t mutually exclusive. In fact, the 2023 Dry Eye Workshop II report recommends combining cyclosporine with punctal plugs for severe cases. Why? Because one fixes the cause, the other conserves the result. One study showed this combo improved symptoms 78% more than either alone.
What Doctors Really Recommend
According to the American Optometric Association, cyclosporine is still the first-line treatment for moderate to severe dry eye. Why? Because it’s the only one proven to heal the eye surface over time. But not everyone can tolerate it. The burning, the cost, the wait - they’re real barriers. That’s why many doctors start patients on lifitegrast if they need faster relief, or if they’ve already tried cyclosporine and quit.
Optometrists are more likely to use plugs early, especially if your Schirmer’s test (a simple tear measurement) shows you’re making less than 10mm of tears in five minutes. Ophthalmologists tend to wait longer, preferring to try medications first. But if you’ve tried drops for months with no improvement, plugs are a logical next step.
Here’s a real-world flow many clinics follow:
- Start with over-the-counter drops and lifestyle changes (screen breaks, humidifiers, omega-3s).
- If no improvement in 4-6 weeks, try cyclosporine.
- If burning is too bad or no improvement after 3 months, switch to lifitegrast.
- If symptoms persist, consider punctal plugs - especially if tear production is low.
- For stubborn cases, combine cyclosporine + plugs.
And yes, some people end up on all three - cyclosporine in the morning, lifitegrast at night, and plugs in place for months. It’s not ideal, but for some, it’s the only way to get through the day without reaching for a bottle of drops every hour.
What You Can Do Right Now
If you’re considering these treatments, here’s what to do:
- Ask for a Schirmer’s test - it tells you if your tear production is low. If it’s under 10mm, plugs are worth discussing.
- Don’t quit cyclosporine too soon - most people give up before 3 months. Keep a journal: note burning, clarity, screen comfort. You might be surprised by month 4.
- Store Restasis in the fridge - it reduces the burning sensation. Many users swear by this trick.
- Use Xiidra at night - if you get the metallic taste, taking it before bed helps you sleep through it.
- Check for patient assistance programs - Restasis has one covering 78% of insured patients. Xiidra offers a $0 co-pay for the first month.
- Don’t use drops with plugs - unless your doctor says otherwise. Too many drops can push plugs out.
And if you’re wondering about new options - yes, they’re coming. A once-daily version of lifitegrast (Vevye) is in late-stage trials. Collagen plugs that release cyclosporine slowly (Cyclplug) are being tested in Europe. But for now, the three you know are still the main tools.
Final Thoughts
Dry eye isn’t just an annoyance. It’s a chronic condition that can affect your work, your driving, your quality of life. There’s no one-size-fits-all fix. Cyclosporine is slow but healing. Lifitegrast is fast but temporary. Plugs are mechanical and reliable - but not a cure.
The best outcome? A plan that matches your symptoms, your lifestyle, and your patience. If you’re willing to wait, cyclosporine might be your best long-term bet. If you need relief now, lifitegrast gives you a fighting chance. And if your eyes just can’t hold onto tears? Plugs might be the quiet hero you didn’t know you needed.
Don’t settle for drops that don’t work. Talk to your eye doctor. Ask for the numbers. Ask for options. You deserve to see clearly - without burning, without blinking, without begging for relief.
How long does it take for cyclosporine to work for dry eye?
Cyclosporine typically takes 3 to 6 months to show full effect. Some people notice slight improvement after 4 weeks, but consistent use for at least 90 days is needed to see real healing of the eye surface. Stopping early means losing any benefit.
Does lifitegrast cause a bad taste? Can I avoid it?
Yes, about 42% of users report a metallic or bitter taste after using Xiidra. It’s not dangerous, but it’s unpleasant. The best way to reduce it is to use the drops at night before bed. Some people also find that closing their eyes for 30 seconds after applying helps minimize the taste reaching the throat.
Are punctal plugs permanent?
No - but they can be. Collagen plugs dissolve in 3 to 10 days and are used for testing. Silicone plugs are designed to stay in permanently, but they can be removed if needed. About 28% of patients experience plug extrusion, meaning the plug falls out on its own, especially in the first few weeks.
Can I use over-the-counter drops with cyclosporine or lifitegrast?
Yes, but not at the same time. Wait at least 15 minutes after using cyclosporine or lifitegrast before applying any artificial tears. This gives the prescription medicine time to absorb. Using them together can wash out the active ingredient.
Is there a cheaper alternative to Restasis or Xiidra?
Yes. Generic cyclosporine (0.05%) is now available as single-use vials and costs about half the price of brand-name Restasis. There is no generic version of Xiidra yet, but some patients switch to generic cyclosporine after trying Xiidra and find it just as effective for long-term use.
What happens if punctal plugs fall out?
If a plug falls out, it’s not dangerous - your eyes just return to their previous state. Temporary plugs are meant to dissolve. Silicone plugs can be easily reinserted by your eye doctor. If they keep falling out, your doctor may try a larger size or switch to a different material. Some patients benefit from permanent plugs placed deeper in the duct.
Can I wear contact lenses with these treatments?
You should remove contact lenses before applying cyclosporine or lifitegrast. Wait at least 15 minutes after using either medication before reinserting lenses. Many patients find that dry eye treatments make contacts more comfortable over time - but only if used correctly.


LIZETH DE PACHECO
January 2, 2026 AT 20:26I tried Restasis for 5 months and almost quit at month 3-burning felt like my eyes were full of glitter. But then, outta nowhere, my contacts stopped sticking. Now I don’t even need drops by afternoon. Just don’t give up before the magic kicks in.
Lee M
January 4, 2026 AT 13:57Let’s be real-Big Pharma doesn’t care if your eyes burn. They care that you keep buying $600 bottles. Cyclosporine? It’s not healing your eyes, it’s just numbing the inflammation while they patent the next overpriced drop. Wake up. The real cure is reducing screen time, not injecting immunosuppressants into your corneas.
Kristen Russell
January 5, 2026 AT 03:52Xiidra gave me that weird metal taste so bad I almost threw up. But I started using it right before bed-and now I don’t even notice it. Game changer.
Bryan Anderson
January 6, 2026 AT 07:09Thank you for this thorough breakdown. I’ve been on cyclosporine for four months and was beginning to doubt its efficacy. Your mention of the JAMA study gave me renewed motivation to continue. I’ve also started using a humidifier at night-small changes, but they’re helping.
Matthew Hekmatniaz
January 6, 2026 AT 12:06In India, we use rosewater and warm compresses for dry eyes-simple, cheap, and passed down for generations. Not a replacement for meds, but a nice complement. I’ve seen people in rural clinics with no access to Restasis still managing decent eye comfort with just clean cloths and patience. Sometimes the oldest remedies hold the quietest wisdom.
Liam George
January 8, 2026 AT 08:00Did you know the FDA approved Restasis after a 12-month trial funded by Allergan? The placebo group had higher rates of ‘improvement’ in early phases, but they changed the endpoint at the last minute. And now you’re told to use it twice daily for six months? That’s not medicine-that’s behavioral conditioning. They want you addicted to the ritual. Plugs? They’re just temporary fixes while they wait for you to sign up for the next ‘breakthrough’ drug. Wake up. The tear ducts weren’t meant to be plugged. Nature didn’t design them to drain-your body is trying to tell you something.
sharad vyas
January 8, 2026 AT 17:35My uncle in Delhi had dry eyes for 10 years. He stopped using drops after his glasses broke. Started blinking slowly on purpose, looked away from screens every 20 minutes, drank more water. Now he says his eyes feel ‘lighter.’ Not cured, but better. Maybe the answer isn’t always in the bottle.
Bill Medley
January 8, 2026 AT 21:59For patients considering punctal plugs, I recommend a diagnostic trial with collagen plugs prior to silicone insertion. This minimizes unnecessary procedures and allows for objective assessment of therapeutic benefit.
Richard Thomas
January 10, 2026 AT 03:26It’s fascinating how we’ve come to treat a natural physiological response-dry eyes-as a disease to be medicated rather than a symptom of modern life. We stare at screens 10+ hours a day, breathe dry air in climate-controlled buildings, and then wonder why our tear film evaporates faster than a puddle in the desert. Cyclosporine and lifitegrast are Band-Aids on a bullet wound. We’re treating the symptom while ignoring the systemic cause: our attention economy. The real solution isn’t a prescription-it’s a lifestyle recalibration. Reduce screen time. Blink consciously. Take walks outside. Let your eyes rest. The body heals when given space. We’ve forgotten that. We’ve outsourced healing to pharmaceuticals because it’s easier than changing our habits. But ask yourself: if you had to live without these drops for a year, could you? Or are you just afraid of what your eyes would say if you finally stopped ignoring them?