Blood Calcium Levels: What They Mean and How to Manage Them
Blood calcium is one of those numbers your doctor watches closely. It affects your nerves, muscles, bones, and heartbeat. If your calcium is outside the normal range, you can feel anything from mild fatigue to severe muscle spasms or confusion. This page explains the numbers, common causes, simple tests, and practical next steps.
What are normal calcium levels?
Most labs report total serum calcium. A typical range is about 8.5–10.2 mg/dL. If your albumin is low, your total calcium can look low even when the active (ionized) calcium is fine. Doctors often use a correction: corrected Ca = measured Ca + 0.8 × (4.0 − albumin in g/dL). Ionized calcium—the biologically active form—usually runs near 4.6–5.3 mg/dL and is measured when accuracy matters.
Why calcium can be too low or too high
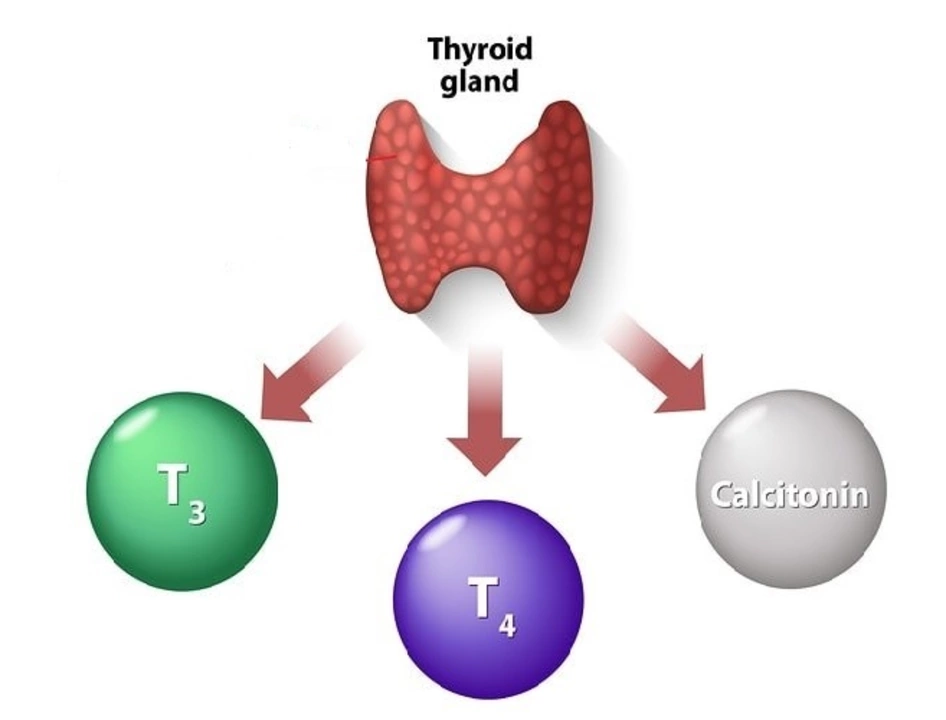
Low calcium (hypocalcemia) shows up with numbness or tingling around the mouth, muscle cramps, twitching, or even severe cramps and seizures. Common causes include low parathyroid hormone (after neck surgery or autoimmune disease), vitamin D deficiency, kidney failure, low magnesium, and certain meds like bisphosphonates or some chemotherapy drugs.
High calcium (hypercalcemia) often causes tiredness, thirst, frequent urination, constipation, and bone or stomach pain. Major causes are overactive parathyroid glands (primary hyperparathyroidism), some cancers that affect bones or release calcium, too much vitamin D, certain medications (thiazide diuretics), and prolonged immobility.
Symptoms can overlap or be subtle. Mild abnormalities sometimes cause no obvious signs, so lab tests matter.
Tests and what to expect
Your doctor will usually start with a basic metabolic panel or specific serum calcium test. If total calcium is off, they may check albumin, ionized calcium, parathyroid hormone (PTH), vitamin D, magnesium, kidney function, and sometimes urine calcium. These tests tell whether the issue is coming from the parathyroid glands, kidneys, vitamin D status, or another cause.
Severe hypocalcemia (numbness, cramping, spasms, or cardiac changes) is treated urgently with IV calcium, usually calcium gluconate. Mild cases often respond to oral calcium supplements plus vitamin D (or active vitamin D like calcitriol if PTH is low). For hypercalcemia, the immediate steps are fluids and monitoring; treatments can include IV fluids, diuretics, bisphosphonates, or medications that lower PTH, depending on the cause.
Practical tips: keep well hydrated, don’t take high-dose calcium supplements unless your doctor recommends them, check vitamin D and magnesium if your calcium is weird, and ask for a corrected calcium or ionized calcium test if albumin is low. If you have chest pain, severe weakness, fainting, or seizures, seek emergency care right away.
If your labs show abnormal calcium, work with your clinician to find the cause. Treating the root problem—parathyroid disease, vitamin D issues, kidney problems, or cancer—usually fixes calcium too. Regular follow-up labs help track progress and keep your heart and nerves safe.