Calcitonin: What It Does and When It's Used
Calcitonin is a hormone medicine that helps lower blood calcium and slows bone breakdown. Doctors use it for certain cases of high calcium and for bone conditions like osteoporosis or Paget's disease when other treatments aren't suitable. It works fast enough to be useful in urgent situations, but it's not a cure-all. This page gives straight answers about how calcitonin works, how people take it, and what to watch for.
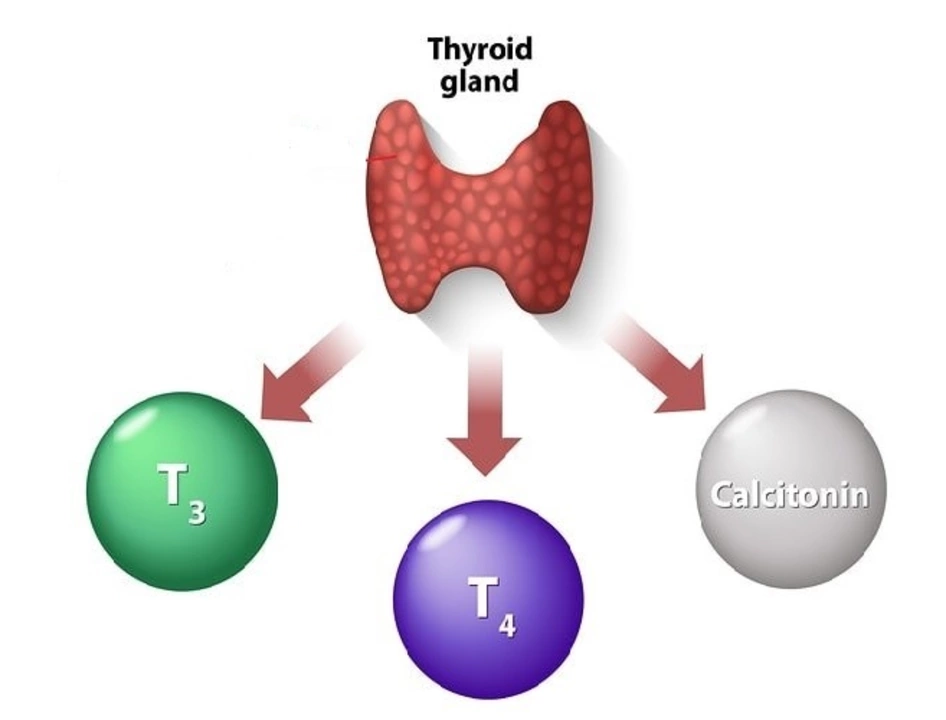
What calcitonin is and how it works
Calcitonin is similar to a natural hormone made by the thyroid gland. It tells bones to stop releasing calcium into the blood and tells the kidneys to excrete more calcium. That dual action lowers blood calcium levels and can reduce bone loss over time. The drug form comes from salmon or human-made versions; salmon-derived calcitonin is more common because it's stronger and lasts longer in the body.
Because it acts differently from drugs like bisphosphonates or denosumab, calcitonin can be an option when those treatments aren't possible — for example, if someone can’t tolerate the side effects of other medicines or needs a short-term fix for high calcium.
Uses, dosing, and safety
Common uses: treating hypercalcemia (high blood calcium), managing osteoporosis in some patients, and easing bone pain from Paget's disease. Forms available: injectable solution and a nasal spray. Injection is usually used in hospital settings for fast control of calcium. The nasal spray is more common for longer-term bone support but is less powerful.
Dosing varies. For high calcium, hospitals give injections under monitoring. For osteoporosis, patients often use a daily or alternate-day nasal spray. Always follow your prescriber's exact instructions and never switch forms or doses without asking them.
Side effects to expect: nausea, flushing, local irritation with nasal spray, and injection-site reactions. Rare but serious reactions can include allergic responses—especially with salmon-derived calcitonin—so tell your doctor if you have fish allergies. Long-term use may carry small risks; recent guidance limits routine long-term use for osteoporosis because better options exist now.
Talk to your doctor before starting calcitonin if you are pregnant, breastfeeding, have low calcium, kidney problems, or known allergies. Watch calcium levels and kidney function as advised. If you notice severe rash, trouble breathing, or sudden swelling, seek medical help right away.
Storage and handling are simple: keep injections and sprays in their original packaging, follow refrigeration or room-temperature instructions, and check expiration dates. If you have questions about dose timing, missed doses, or combining calcitonin with vitamins or other bone medicines, ask your healthcare team — they’ll tailor advice to your situation.
Want more detail or patient-friendly resources? Reach out to your pharmacist or doctor — they can explain how calcitonin fits into your overall treatment plan and help you avoid common mistakes.