Osteomyelitis: What You Need to Know About Bone Infection
Osteomyelitis means an infection inside a bone. It can start quickly after an injury or surgery (acute) or smolder for months or years (chronic). If you have unexplained bone pain, fever, or a wound that won’t heal near a bone, don’t ignore it — early care makes a big difference.
How it starts and who’s at risk
The most common germ is Staphylococcus aureus, but other bacteria and rarely fungi can cause it. Infections reach bone in three main ways: bacteria traveling in the blood, spread from a nearby infected wound, or direct entry after a fracture or surgery. People with diabetes, poor circulation, weakened immune systems, IV drug use, or implanted metal hardware (like screws or plates) are at higher risk.
Signs, diagnosis, and tests
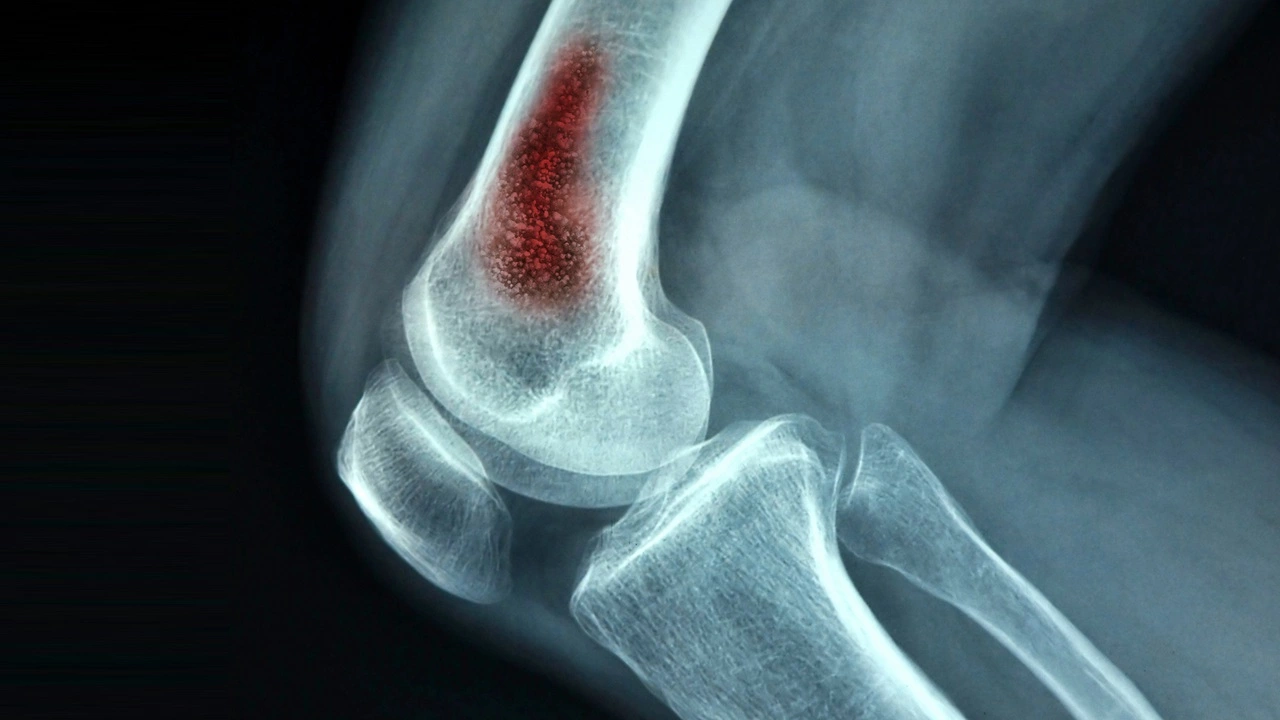
Typical symptoms are steady, deep bone pain, swelling, redness over the area, fever, and sometimes pus draining from a wound. In chronic cases the pain can be milder and a draining sinus may be the only sign. Doctors check blood markers (CRP, ESR, white blood cell count) and try to get blood cultures. Plain X-rays can miss early disease; MRI is the most sensitive test for seeing infected bone and nearby soft tissue. Bone scan or PET can help when MRI isn’t possible. The best way to identify the exact germ is a bone biopsy or surgical sample — that guides targeted antibiotics.
Treatment aims to remove the infection and save as much bone and function as possible. Most people need IV antibiotics for several weeks — often 4–6 weeks, sometimes longer for chronic cases. After IV therapy, doctors may switch to oral antibiotics based on the bug and how you respond. If there’s dead bone, a large abscess, or infected hardware, surgery to remove damaged tissue and drain pus is common. For some chronic cases, long-term suppressive antibiotics are used when full cure isn’t possible.
Other helpful measures include good wound care, controlling blood sugar if you have diabetes, and physical therapy after healing to restore strength and mobility. Hyperbaric oxygen therapy can help in selected cases, but it’s not routine.
Watch for complications: untreated osteomyelitis can cause sepsis, bone destruction, fractures, and failure of nearby implants. Quick action improves outcomes — stable vitals, shrinking pain, and falling CRP/ESR are signs treatment is working.
If you have a deep, persistent bone pain, a non-healing wound near bone, fever, or recent surgery or fracture with worsening symptoms, contact your doctor or go to urgent care. Early diagnosis and targeted treatment give the best chance to clear the infection and keep your bone healthy.