Renal failure
Renal failure means your kidneys can't do their job: filter waste, balance fluids, and keep electrolytes steady. It can come on fast (acute) or slowly over months to years (chronic). Knowing the difference matters because treatment and outlook change.
Spotting it early
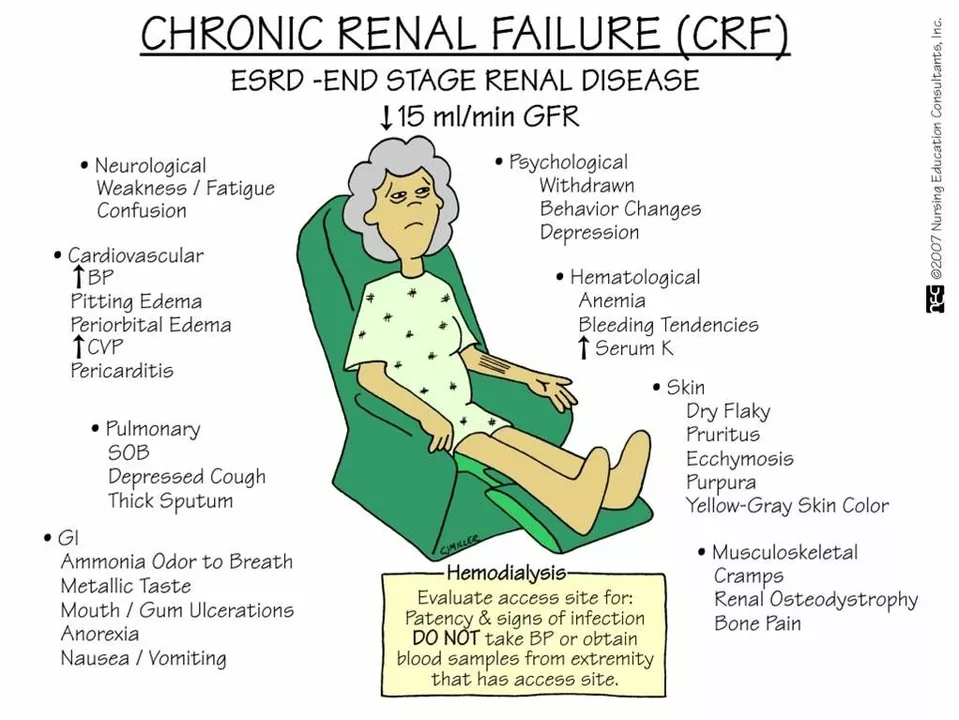
Common signs include less urine or darker urine, swelling in ankles and face, constant tiredness, nausea, loss of appetite, and shortness of breath. Some people notice no symptoms until the problem is advanced. Blood tests (creatinine, eGFR) and urine tests show how well kidneys work. Imaging or a kidney biopsy may be needed to find the cause.
Causes and common triggers
Acute kidney injury often follows severe dehydration, major infection, a drop in blood pressure, or certain drugs (NSAIDs, some antibiotics, contrast dye). Chronic kidney disease usually comes from long-standing problems like diabetes, high blood pressure, repeated urinary infections, or inherited disorders. If you take multiple medicines, ask your doctor or pharmacist whether any could harm your kidneys.
Treatment depends on the cause and how bad the damage is. For acute injury, fixing the underlying issue—rehydration, treating infection, adjusting meds—can let kidneys recover. Chronic disease focuses on slowing decline: control blood sugar and blood pressure, reduce protein in the urine, treat anemia and bone-mineral problems, and avoid toxins. Your care team may include a nephrologist, dietitian, and pharmacist.
If kidneys fail to maintain function, dialysis or kidney transplant become options. Dialysis removes waste and extra fluid; there are dialysis machines at centers or home options. Transplant offers a return to more normal life for many, but it requires lifelong medications to prevent rejection. Talk to your specialist about timing—early education improves outcomes.
Simple steps can protect your kidneys: keep blood pressure and blood sugar in target, stay hydrated without overdoing it, avoid unnecessary NSAIDs and certain supplements, and get yearly kidney checks if you have diabetes or hypertension. Watch salt intake and aim for protein and fluid guidance from a dietitian—what's right varies by stage.
If you notice sudden drops in urine output, severe swelling, confusion, or breathlessness, seek urgent care. For gradual symptoms—fatigue, poor appetite, ankle swelling—make a primary care appointment and ask for kidney function tests. Bring a list of all medications and supplements; many kidney problems are linked to drug exposure.
Common medicines that can harm kidneys include high-dose NSAIDs (like ibuprofen or naproxen), certain antibiotics such as aminoglycosides, and some heart medicines when blood pressure drops too low. Herbal supplements aren't always safe; tell your doctor what you take. Regular reviews of medicines—especially if you're older or have diabetes—cut risk. Ask your pharmacist about dosing after kidney damage. Small checks and honest talk with your team make a big difference.
Resources and links are on PharmNet for patients.