Bipolar Episode Risk Checker
Symptom Assessment Tool
Answer the questions below to assess potential risk of mania or depression. This tool is for awareness only - not a diagnosis.
Risk Assessment Results
Mania Indicators Detected
You're showing signs of potential mania. This may include:
- Elevated mood or irritability
- Reduced need for sleep
- Racing thoughts or impulsivity
Depression Indicators Detected
You're showing signs of potential depression. This may include:
- Persistent sadness or emptiness
- Loss of interest in activities
- Fatigue or low energy
Immediate Help Needed
If you're experiencing suicidal thoughts or unsafe behavior, please:
- Call emergency services immediately
- Go to your nearest emergency room
- Text 988 or call 1-800-273-TALK (8255) in the US
You're not alone - help is available right now.
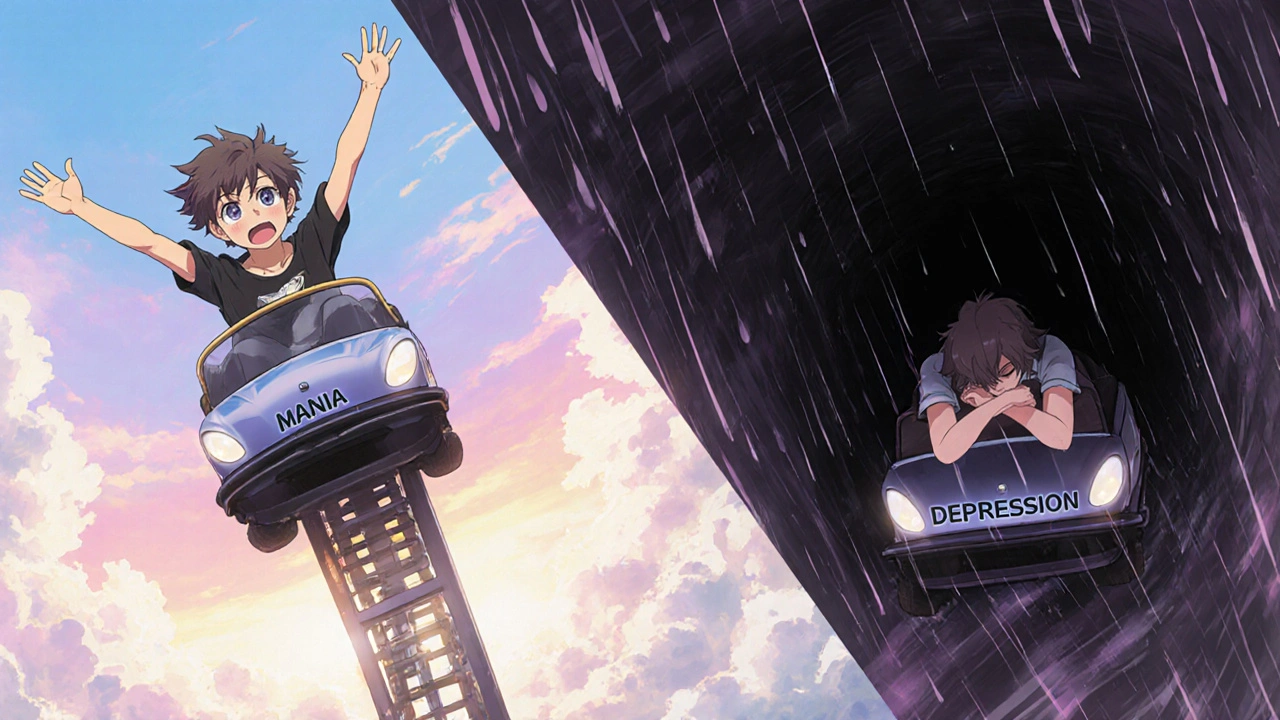
When mood swings swing from sky‑high to rock‑bottom, it can feel like an emotional roller coaster you never signed up for. Bipolar disorder is a mental health condition marked by recurring manic and depressive episodes that disrupt daily life, relationships, and work. Recognizing the early clues can mean the difference between a manageable flare‑up and a crisis that spirals out of control.
What Counts as a Mood Episode?
In the world of bipolar disorder, clinicians break down the experience into two distinct phases:
- Manic episode is a period of unusually elevated, expansive, or irritable mood that lasts at least one week (or less if hospitalization is needed).
- Depressive episode is a stretch of low mood, loss of interest, and a drop in energy that sticks around for at least two weeks.
Both phases can sneak in gradually, but each has a signature set of warning signs you can learn to spot.
Why Early Detection Matters
Spotting the first hints lets you act before the episode fully takes hold. Early intervention has been shown to reduce hospital stays by up to 30 % and improves long‑term functioning (National Institute of Mental Health, 2024). It also gives you and your support network time to put coping tools in place, rather than scrambling in crisis mode.
Warning Signs of a Manic Episode
Mania isn’t just feeling “good.” It’s an over‑the‑top surge that can impair judgment. Keep an eye out for these red flags:
- Racing thoughts that jump from one idea to the next, making it hard to finish a sentence.
- Inflated self‑esteem or grandiosity - believing you’re capable of things that are unrealistic.
- Reduced need for sleep - feeling refreshed after only a few hours.
- Talkativeness that borders on pressure to keep speaking, often louder than usual.
- Increased goal‑directed activity: starting many projects, spending sprees, or risky sexual behaviour.
- Distractibility - easily pulled away by irrelevant stimuli.
- Impulsivity - making snap decisions without weighing consequences.
Warning Signs of a Depressive Episode
Depression can feel like a heavy blanket you can’t shake off. Typical early indicators include:
- Persistent sadness, emptiness, or hopelessness that lasts most of the day.
- Loss of interest in hobbies, friends, or work that once brought joy.
- Significant changes in appetite - either eating far more or far less.
- Sleep disturbances - insomnia, early‑morning awakening, or oversleeping.
- Fatigue or loss of energy, even after adequate rest.
- Feelings of worthlessness or excessive guilt about past actions.
- Difficulty concentrating, making decisions, or remembering details.
- Thoughts of death or suicide - any mention of self‑harm should be taken seriously.

How to Differentiate Overlapping Signs
Some symptoms-like sleep changes or irritability-appear in both mania and depression. The key is to look at the direction of the change:
- Sleep: Mania = dramatically less sleep; Depression = insomnia or oversleeping.
- Energy: Mania = hyper‑active, wired; Depression = lethargic, slowed down.
- Mood tone: Mania = elevated or irritable; Depression = sad or empty.
When in doubt, track the pattern for a few days. A simple mood diary can reveal whether the swings are heading toward mania or depression.
Action Plan: What to Do When You Notice the Signs
- Pause and record: Note the specific behaviors, timing, and any triggers. A phone note or journal works.
- Reach out early: Call a trusted friend, family member, or therapist. Early conversation often de‑escalates the episode.
- Check your medication: If you’re already on mood stabilizers, verify you’ve taken them as prescribed. Missing doses is a common precipitant.
- Use coping tools: Practice grounding techniques (deep breathing, 5‑4‑3‑2‑1 sensory check), stick to a regular sleep schedule, and limit caffeine or stimulants.
- Seek professional help: If signs intensify, schedule an urgent appointment with a psychiatrist or go to an emergency department.
Support Network Tips
Family and friends play a crucial role. Here’s how they can help without sounding judgmental:
- Ask open‑ended questions: “I’ve noticed you’ve been very energetic lately-how are you feeling?”
- Avoid labels: Instead of “You’re acting crazy,” say “I’m concerned about the changes I’m seeing.”
- Offer concrete assistance: “Would you like me to drive you to your doctor’s appointment?”
- Set gentle boundaries: If risky spending starts, suggest a shared budgeting app.
Treatment Options Overview
While spotting signs is vital, treatment keeps the episodes in check. The standard toolkit includes:
- Mood stabilizers: Lithium, valproate, and lamotrigine are first‑line for preventing both mania and depression.
- Atypical antipsychotics: Quetiapine and aripiprazole help when mood stabilizers aren’t enough.
- Antidepressants: Used cautiously, often combined with a mood stabilizer to avoid triggering mania.
- Psychotherapy: Cognitive‑behavioral therapy (CBT) and dialectical behavior therapy (DBT) teach coping skills and relapse prevention.
- Lifestyle interventions: Regular exercise, balanced diet, and consistent sleep hygiene reduce episode frequency.

Daily Habits for Long‑Term Stability
Even with medication, everyday choices matter. Try these evidence‑based habits:
- Maintain a fixed sleep‑wake schedule-aim for 7‑9 hours.
- Limit caffeine after 2 p.m. and avoid alcohol binge‑drinking.
- Engage in moderate aerobic exercise at least three times a week; studies show a 20 % reduction in depressive symptoms.
- Use a mood‑tracking app (e.g., MoodChart) to spot patterns early.
- Schedule regular check‑ins with your therapist-monthly is a good baseline.
Quick Comparison: Manic vs. Depressive Signs
| Warning Sign | Manic Episode | Depressive Episode |
|---|---|---|
| Sleep | Significantly reduced (often < 4 hrs) | Insomnia or oversleeping |
| Energy | Hyper‑active, pressured | Fatigue, slowed movements |
| Mood | Euphoric, irritable, grandiose | Sad, hopeless, empty |
| Thoughts | Racing, disorganized | Negative, hopeless |
| Risky behavior | Spending sprees, reckless driving | Withdrawal, self‑harm ideation |
When to Call Emergency Services
If you or someone you know shows any of the following, treat it as a medical emergency:
- Talk of suicide, self‑injury, or a specific plan.
- Severe agitation that could lead to harm.
- Hallucinations or delusional thinking that impair safety.
- Inability to care for basic needs (eating, dressing) for more than 24 hours.
Dial 911 or go to the nearest emergency department. Prompt care can prevent a full‑blown crisis.
Frequently Asked Questions
Can I have both manic and depressive symptoms at the same time?
Yes. A mixed episode features simultaneous manic and depressive features, making it harder to identify. Look for high energy paired with deep sadness or irritability. Mixed states require immediate professional evaluation.
How long do warning signs usually appear before a full episode?
Early warning signs can show up days to weeks before the episode peaks. Recognizing subtle changes-like a slight dip in sleep or a minor increase in spending-offers a window for early intervention.
Do lifestyle changes alone prevent episodes?
Lifestyle tweaks (regular sleep, exercise, stress management) dramatically lower relapse risk, but they are most effective when combined with medication and therapy. Skipping medication in favor of lifestyle alone can increase the chance of a severe episode.
Is it normal to feel “normal” after a period of mania or depression?
Many people experience a “baseline” period that feels stable, but it’s still part of the bipolar cycle. Regular monitoring is key because the next episode can start subtly.
What should family members do if they suspect a loved one is entering a manic phase?
Start a calm conversation, express concern without blame, and suggest a medication check or therapist visit. Offering concrete help-like setting up a doctor’s appointment-often works better than vague “you need to calm down” remarks.
By learning these warning signs, tracking mood changes, and acting early, you give yourself or your loved one the best shot at staying balanced and avoiding the worst‑case scenarios of bipolar disorder.

Erika Thonn
October 21, 2025 AT 15:53When you stare into the abyss of a shifting mind, you begin to hear the subtle drumbeat of destiny that many ignore. The first whisper of mania may feel like a sunrise that never sets, a promise of boundless power that tempts the soul. Yet beneath that glitter lies a fault line, a fissure that can split the self if left unchecked. Similarly, the shadows of depression creep in like a fog, muffling the colors of life and stealing the fire from ordinary moments. In the ancient texts, philosophers warned that awareness precedes mastery; knowing the signs is the first step toward controlling the tempest. Ignoring early cues is akin to sailing blind into a storm, trusting only the wind to guide you. The list of symptoms – racing thoughts, reduced sleep, grandiosity – each is a beacon that flickers when the mind tilts toward excess. When you notice a sudden surge of invincibility, pause and ask: is this truly me or a masquerade? The same applies when the weight of hopelessness settles like concrete on your chest; recognize the heaviness before it becomes a cage. Record these moments in a journal, for the act of writing anchors the wandering mind. A simple note about a missed night’s sleep can later reveal a pattern that warns of an impending episode. Knowledge, however, is not static; it must be rehearsed like a mantra, repeated until it becomes second nature. In this way, the individual becomes a steward of their own mental weather, adjusting sails before the gale. The community around you, too, can serve as a mirror, reflecting back the changes you might miss in your own reflection. Ultimately, early detection transforms chaos into a dance, where each step is guided by insight rather than panic. Embrace the practice, and you will find the roller coaster of bipolar becomes something you can ride with eyes wide open.
Ericka Suarez
November 9, 2025 AT 06:10Honestly this article is like a beacon for the american spirit, it shows how we can take control of our own minds! The warning signs are crystal clear, you cant miss them if you pay attention. Manic episodes feel like a fireworks show, bright and loud, but you gotta remember the fallout. Depressive dives are like a dark tunnel, but we can light it with proper tools. Its so simple, you just have to track your sleep and mood, no rocket science involved. I love how they give practical steps, like reaching out early, that just shows common sense. The whole thing feels like a reminder that we are stronger than any mental storm. Keep this info coming, we need more of this kind of guidance for real americans!
Jake Hayes
November 27, 2025 AT 21:26Spotting early signs saves time and reduces risk. Track sleep, mood, energy. Use a diary. Reach out before escalation.
parbat parbatzapada
December 16, 2025 AT 13:00They think a simple diary will stop the brain from being hijacked by hidden forces. Ever wonder why the pharma giants push meds so hard? The real danger is the surveillance state watching our moods, feeding data to control us. Trust no one but yourself, and keep your thoughts private.
Casey Cloud
January 4, 2026 AT 04:33When you notice a change in sleep patterns try setting an alarm to remind you to log your mood it helps to have a visual cue and you can share the notes with a therapist they will appreciate the detail
Rachel Valderrama
January 22, 2026 AT 20:06Wow, because we all just love waking up at 3 am and writing novels in our heads.
Brandy Eichberger
February 10, 2026 AT 11:40Hey there! I think the guide does a wonderful job of breaking down complex concepts into bite‑size, friendly pieces. It’s like having a gentle mentor whispering practical tips over a cup of tea. Keep sharing such thoughtful resources!