When you start taking an antipsychotic for schizophrenia, bipolar disorder, or severe depression with psychotic features, the goal is clear: calm the voices, reduce the paranoia, bring back some peace. But for many people, that relief comes with a hidden cost-weight gain, high blood sugar, rising cholesterol, and a growing risk of heart disease and diabetes. These aren’t rare side effects. They’re common, serious, and often ignored.
Why Some Antipsychotics Change Your Body Chemistry
Second-generation antipsychotics (SGAs), like olanzapine, clozapine, and quetiapine, were designed to be safer than older drugs by reducing muscle stiffness and tremors. But in the early 2000s, researchers started seeing a pattern: patients on these meds were gaining weight fast, developing prediabetes, and showing abnormal cholesterol levels-even before they gained much weight. This wasn’t just about eating more. The drugs themselves were messing with how the body processes sugar and fat. The biggest culprits are olanzapine and clozapine. In the CATIE study, people on olanzapine gained an average of 2 pounds per month during the first year. About 30% gained 7% or more of their body weight. Clozapine isn’t far behind. Both drugs strongly block histamine and serotonin receptors in the brain, which increases hunger and slows metabolism. Even people who don’t gain weight can develop insulin resistance. That means their bodies can’t use insulin properly, leading to high blood sugar-even if they’re thin. On the other end of the spectrum, aripiprazole, ziprasidone, and lurasidone have much lower metabolic risks. Aripiprazole, for example, causes weight gain in only about 5% of users. These drugs don’t hit the same brain receptors as hard, so they’re less likely to trigger metabolic chaos. But they’re not always the best choice for symptom control. For treatment-resistant psychosis, clozapine remains the gold standard-even with its risks.What Metabolic Problems You Might Face
The body doesn’t just gain weight. It starts breaking down in other ways too. Here’s what can happen:- Weight gain: Often rapid, especially in the first 6 months. Fat tends to collect around the waist, not just the hips or thighs.
- High blood sugar: Can lead to prediabetes or type 2 diabetes. Some people develop diabetes within a year of starting olanzapine.
- Dyslipidemia: Triglycerides rise, HDL (the good cholesterol) drops. This creates a perfect storm for heart disease.
- High blood pressure: Linked to both weight gain and direct drug effects on blood vessels.
- Metabolic syndrome: This isn’t one condition-it’s a cluster. The International Diabetes Federation defines it as belly fat (waist circumference over 94 cm for men, 80 cm for women) plus two of: high triglycerides, low HDL, high blood pressure, or high fasting glucose.
Up to 68% of people on SGAs develop metabolic syndrome. That’s compared to just 26% in the general population. And it’s not just about feeling bad-it’s about dying younger. People with serious mental illness live 20 to 25 years less than others. About 60% of that gap is due to heart disease and diabetes, often worsened by antipsychotics.
Who’s at Highest Risk?
Not everyone reacts the same way. Some people gain 50 pounds on olanzapine. Others stay the same. Genetics, lifestyle, and existing health play a big role.- Family history: If you have diabetes, heart disease, or obesity in close relatives, your risk goes up.
- Starting weight: People with BMI over 25 before starting meds are more likely to gain weight.
- Age: Younger adults (18-30) tend to gain more weight than older adults.
- Smoking: Smokers on antipsychotics have higher rates of insulin resistance.
- Medication choice: Olanzapine and clozapine are the highest risk. Aripiprazole and ziprasidone are the lowest.
One study found that 42% of patients never had their blood sugar or cholesterol checked after starting antipsychotics. That’s not just negligence-it’s dangerous.

The Monitoring Checklist You Need
The American Psychiatric Association and American Diabetes Association agree: if you’re on an antipsychotic, you need regular metabolic checks. Here’s what should happen:- Before starting: Measure weight, waist size, blood pressure, fasting blood sugar, and lipid panel (cholesterol and triglycerides).
- At 4 weeks: Check weight and blood pressure. If you’ve gained more than 5% of your body weight, talk to your doctor about lifestyle changes or switching meds.
- At 8 and 12 weeks: Repeat blood sugar and lipids. This is when metabolic changes often show up.
- Every 3 months for the first year: Keep tracking weight, blood pressure, and lab values.
- Annually after that: Even if you feel fine, get your blood sugar and cholesterol checked every year.
Waist measurement matters more than weight. A man with a waist over 94 cm or a woman over 80 cm is at higher risk-even if their BMI is normal. Many doctors still don’t measure this. Ask for it.
What to Do If Your Numbers Go Up
Finding out your blood sugar is high or your cholesterol is through the roof doesn’t mean you have to stop your antipsychotic. But it does mean you need a plan.- Switch meds: If you’re on olanzapine or clozapine and gaining weight fast, ask if switching to aripiprazole or lurasidone is possible. You might lose some symptom control, but you might gain your health back. Many patients report feeling more energetic and confident after switching.
- Lifestyle changes: A 2023 study showed that combining diet and exercise with antipsychotic use cut weight gain by half. You don’t need to run marathons. Just 30 minutes of walking five days a week helps. Cut sugary drinks and processed carbs. Focus on whole foods-vegetables, lean protein, nuts, beans.
- Medications to help: Metformin, a common diabetes drug, has been shown to reduce weight gain and improve insulin sensitivity in people on antipsychotics. Some doctors prescribe it preemptively.
- Work with your team: Your psychiatrist should talk to your primary care doctor. Too often, mental health care and physical health care are separated. That’s a recipe for disaster. Ask for a coordinated care plan.
Real Stories, Real Consequences
On Reddit, someone wrote: “I gained 45 pounds on olanzapine in six months. My knees hurt. I couldn’t walk up stairs. I had to switch to aripiprazole-even though it didn’t calm my thoughts as well-because I was scared I’d die of diabetes.” Another person, on a mental health forum, said: “My psychiatrist never checked my blood sugar. I was diagnosed with type 2 diabetes a year after starting risperidone. I had no symptoms. No warning.” But not everyone sees it as a loss. A 2022 survey found that 82% of clozapine users admitted to major weight gain-but still believed it was worth it. Their psychosis was under control. They weren’t in the hospital. They could hold a job. For them, the trade-off made sense. The truth is, there’s no one-size-fits-all answer. But ignoring the numbers? That’s never the answer.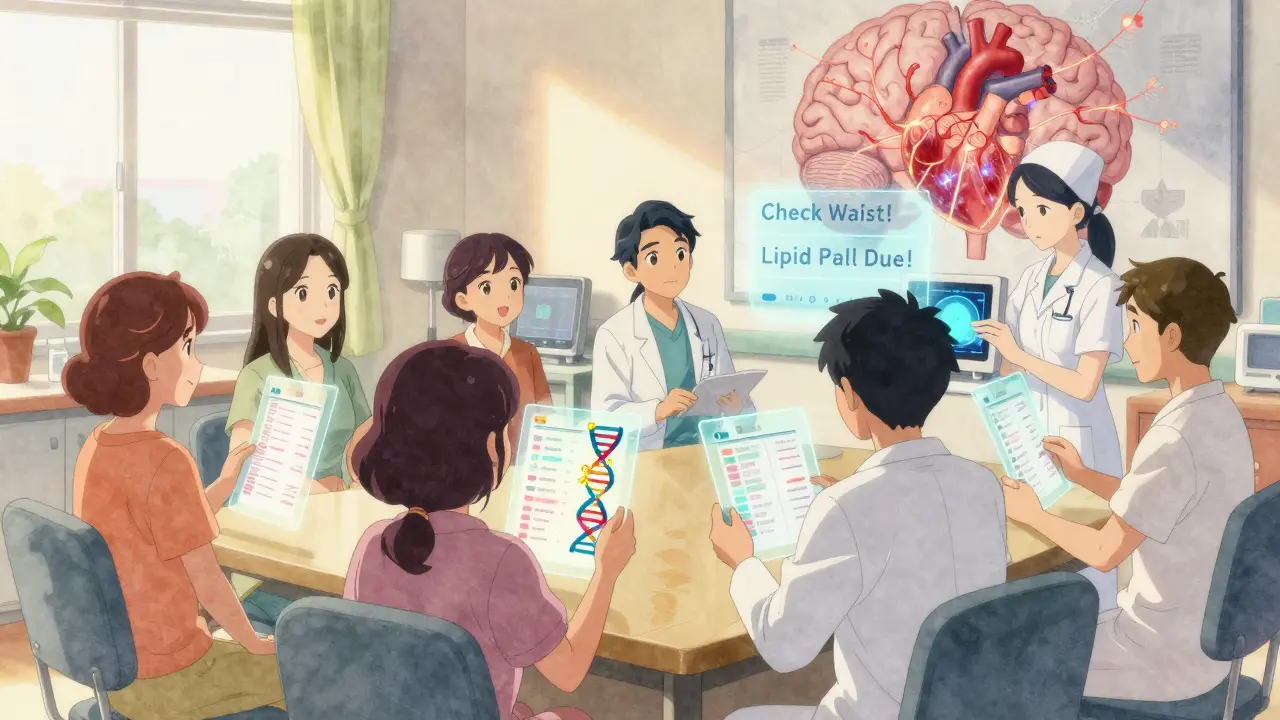
What’s Changing in 2025
The good news? Things are starting to shift. In 2023, the FDA approved lumateperone (Caplyta), a new antipsychotic with minimal weight gain-only 3.5% of users gained weight in trials, compared to 23.7% on olanzapine. It’s not a miracle drug, but it’s a step forward. The National Institute of Mental Health is funding a $12.5 million study to find genetic markers that predict who’s likely to gain weight or develop diabetes on antipsychotics. By 2025, we may be able to test someone’s DNA before prescribing and choose the safest drug from the start. Health systems like Kaiser Permanente have already reduced metabolic complications by 25% by building automated reminders into electronic records. Nurses get alerts when a patient hasn’t had a lipid panel in 12 months. Doctors get prompts to check waist circumference. It’s simple. It works.What You Can Do Today
If you’re on an antipsychotic:- Ask for your baseline labs-weight, waist, BP, fasting glucose, cholesterol. If they haven’t been done, demand them.
- Track your weight weekly. A scale at home is better than waiting for your next appointment.
- Ask your doctor: “Is this the lowest-risk antipsychotic for my situation?”
- If you’re gaining weight fast, don’t wait. Bring up switching meds or adding metformin.
- Find a primary care provider who’s willing to work with your psychiatrist. You need both.
You deserve to be stable mentally-and physically. Antipsychotics save lives. But they shouldn’t shorten them. The tools to protect you exist. You just have to ask for them.
Do all antipsychotics cause weight gain?
No. Weight gain varies widely by medication. Olanzapine and clozapine cause the most-up to 30% of users gain 7% or more of their body weight. Aripiprazole, ziprasidone, and lurasidone have the lowest risk, with weight gain affecting only 5-10% of users. The difference comes down to how each drug interacts with brain receptors that control hunger and metabolism.
Can I avoid metabolic side effects just by eating better and exercising?
Lifestyle changes help, but they’re not always enough. Antipsychotics directly affect how your body processes sugar and fat-even without overeating. Studies show that even with diet and exercise, people on high-risk meds like olanzapine still gain weight faster than those not on medication. The best approach combines healthy habits with medication choice and, if needed, drugs like metformin.
How often should I get blood tests if I’m on an antipsychotic?
Baseline tests should be done before starting. Then check weight and blood pressure at 4 weeks, blood sugar and lipids at 8 and 12 weeks. After that, continue checking every 3 months for the first year, then at least once a year. If you’re on a high-risk drug like clozapine or have other risk factors like obesity or family history of diabetes, your doctor may want more frequent checks.
Is it safe to stop my antipsychotic because of weight gain?
Never stop abruptly. Stopping suddenly can cause psychosis to return worse than before, or trigger withdrawal symptoms like nausea, insomnia, or anxiety. If you’re struggling with side effects, talk to your doctor about switching to a lower-risk medication. Many people successfully transition to aripiprazole or lurasidone without losing symptom control.
Why don’t more doctors monitor metabolic health?
Many psychiatrists are trained to focus on mental symptoms, not physical health. Time is limited in appointments, and electronic health records often don’t remind doctors to check blood sugar or waist size. A 2022 survey found only 38% of U.S. psychiatrists consistently follow monitoring guidelines. But systems that build automated reminders into their records have seen big improvements-so it’s fixable.


Henry Ward
December 31, 2025 AT 07:29This is why I hate how psychiatrists treat patients like lab rats. They slap you on olanzapine like it's candy and then act shocked when you turn into a walking insulin pump. No one talks about how these drugs turn your body against you-and then they wonder why people stop taking them. It's not noncompliance, it's survival.
Kelly Gerrard
December 31, 2025 AT 20:37While I appreciate the clinical rigor of this piece I must emphasize that metabolic monitoring is not optional it is imperative and should be mandated by all psychiatric institutions without exception
Glendon Cone
January 1, 2026 AT 15:08Big thanks for laying this out so clearly 🙏 I was on olanzapine for 2 years and lost 40 lbs after switching to aripiprazole. My knees stopped screaming. My energy came back. It's not about being 'weak'-it's about being smart. Ask for metformin. Ask for waist checks. You deserve both mental peace and physical health.
Aayush Khandelwal
January 3, 2026 AT 05:00Metabolic dysregulation via H1 and 5HT2C receptor antagonism is the primary mechanistic driver here-not merely caloric surplus. The pharmacodynamic footprint of SGAs induces adipogenesis and hepatic insulin resistance independently of behavioral factors. This is why lifestyle interventions alone are insufficient. We need precision prescribing informed by pharmacogenomics.
Sandeep Mishra
January 3, 2026 AT 18:29It's funny how we treat the mind as sacred but the body as disposable. You wouldn't let someone drive a car with a cracked engine and call it 'fine' just because the radio works. Why do we do this with mental health? The body isn't just a vessel-it's the foundation. If it's crumbling, nothing else matters.
Colin L
January 4, 2026 AT 10:22Let me tell you something about these so-called 'low-risk' antipsychotics-aripiprazole? It's a half-baked compromise. Partial agonist? More like partial nonsense. I've seen patients on it still hallucinate while gaining weight because their liver's fried from the damn thing. And don't get me started on lurasidone-expensive, requires food, and still causes akathisia so bad people want to claw their skin off. This whole 'safer alternative' narrative is corporate PR dressed up as science. The truth? There's no safe antipsychotic. Only less terrible ones. And even those come with a side of existential dread.
Hayley Ash
January 4, 2026 AT 15:06Wow what a shocker antipsychotics cause weight gain and diabetes maybe next you'll tell me smoking causes lung cancer
kelly tracy
January 5, 2026 AT 22:03People who say they 'choose' weight gain over psychosis are just brainwashed by the system. They don't realize they're trading their future for temporary calm. I gained 70 pounds. I had to wear adult diapers because my blood sugar crashed so bad I couldn't walk to the bathroom. And now I'm on metformin and still depressed. This isn't treatment. It's slow torture with a side of paternalism.
Nadia Spira
January 6, 2026 AT 22:15It's not the drugs-it's the moral failure of the patient. If you're gaining weight on antipsychotics, you're not trying hard enough. You're eating processed carbs. You're sedentary. You're weak. The system isn't broken-you are. And now you're blaming Big Pharma because you lack discipline. Wake up.
henry mateo
January 6, 2026 AT 23:36i just wanted to say thank you for writing this i was just diagnosed and was terrified but this made me feel like i can fight this. i started walking every day and checking my weight. its scary but i feel less alone now. thanks again
Kunal Karakoti
January 8, 2026 AT 16:04If we accept that the mind and body are inseparable, then prescribing drugs that systematically dismantle metabolic health is not treatment-it's a philosophical contradiction. We are attempting to heal the psyche through methods that corrode the very substrate of life. Perhaps the question isn't which antipsychotic is safest, but whether we should be prescribing any at all without first reconstructing our entire paradigm of care.
srishti Jain
January 8, 2026 AT 18:26My doc didn't check my sugar for a year. I got diabetes. Now I'm on insulin. Thanks for nothing.
Joseph Corry
January 9, 2026 AT 22:17How quaint. You treat metabolic syndrome like a side effect rather than the inevitable consequence of biologically reducing a complex human being to a neurotransmitter equation. The entire psychiatric model is built on control-not healing. You think a lipid panel fixes this? No. You're just measuring the damage while the machine keeps grinding. The real question isn't which drug is safer-it's why we're still using these blunt instruments in the first place.