Hyperkalemia Risk Assessment Tool
Patient Risk Assessment
This tool helps determine your individual risk for hyperkalemia when using ACE inhibitors with spironolactone. Based on guidelines from the article, it provides tailored monitoring recommendations.
Risk Assessment Results
Recommended Monitoring Schedule
Potassium Management Guidance
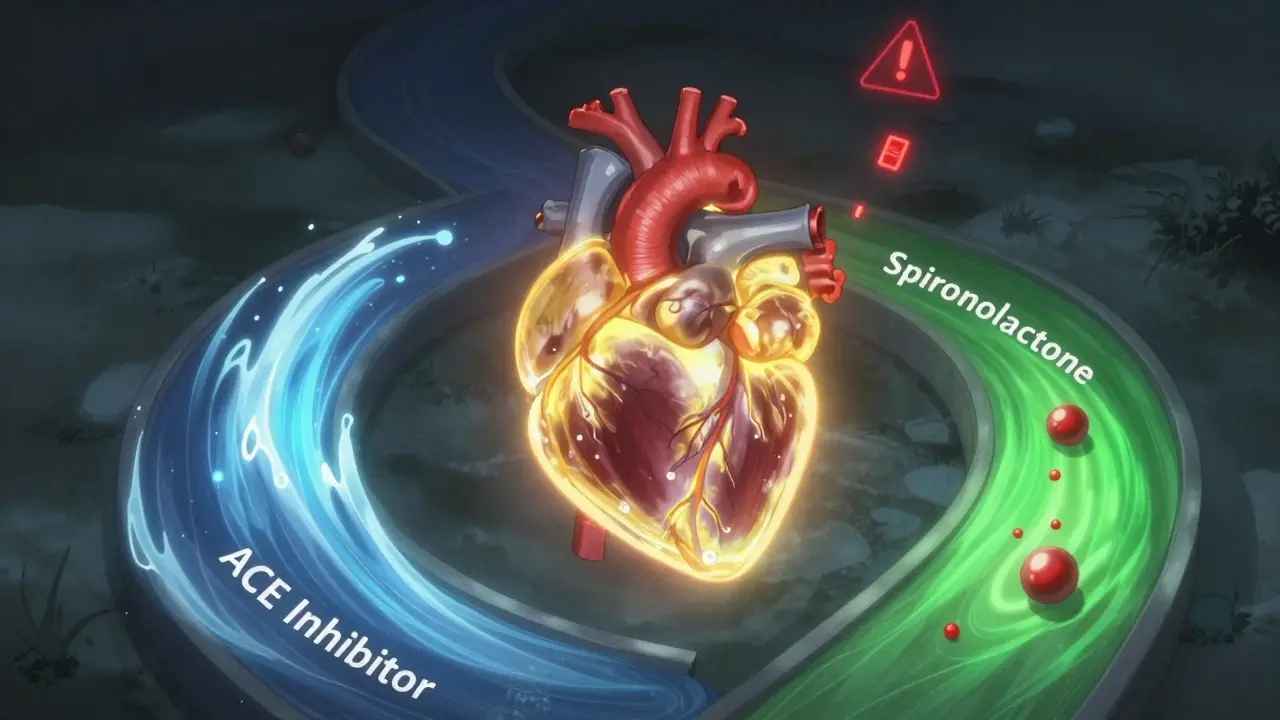
Combining ACE inhibitors and spironolactone can save lives-especially for people with severe heart failure. But it also carries a hidden danger: hyperkalemia, or dangerously high potassium levels. This isn’t just a lab number you ignore. It can trigger irregular heartbeats, cardiac arrest, or even death if left unchecked. Many doctors avoid this combo because of the risk. But newer data shows it’s not about avoiding it entirely-it’s about managing it smartly.
Why This Combo Exists in the First Place
ACE inhibitors like lisinopril or enalapril are common for high blood pressure and heart failure. They work by relaxing blood vessels and reducing strain on the heart. Spironolactone, a diuretic often called a "water pill," blocks the hormone aldosterone. That helps the body get rid of extra fluid and sodium. But here’s the catch: aldosterone also helps the kidneys remove potassium. Block it, and potassium builds up. When you combine the two, you’re hitting potassium excretion from two angles:- ACE inhibitors lower aldosterone production
- Spironolactone blocks aldosterone’s action at the kidney
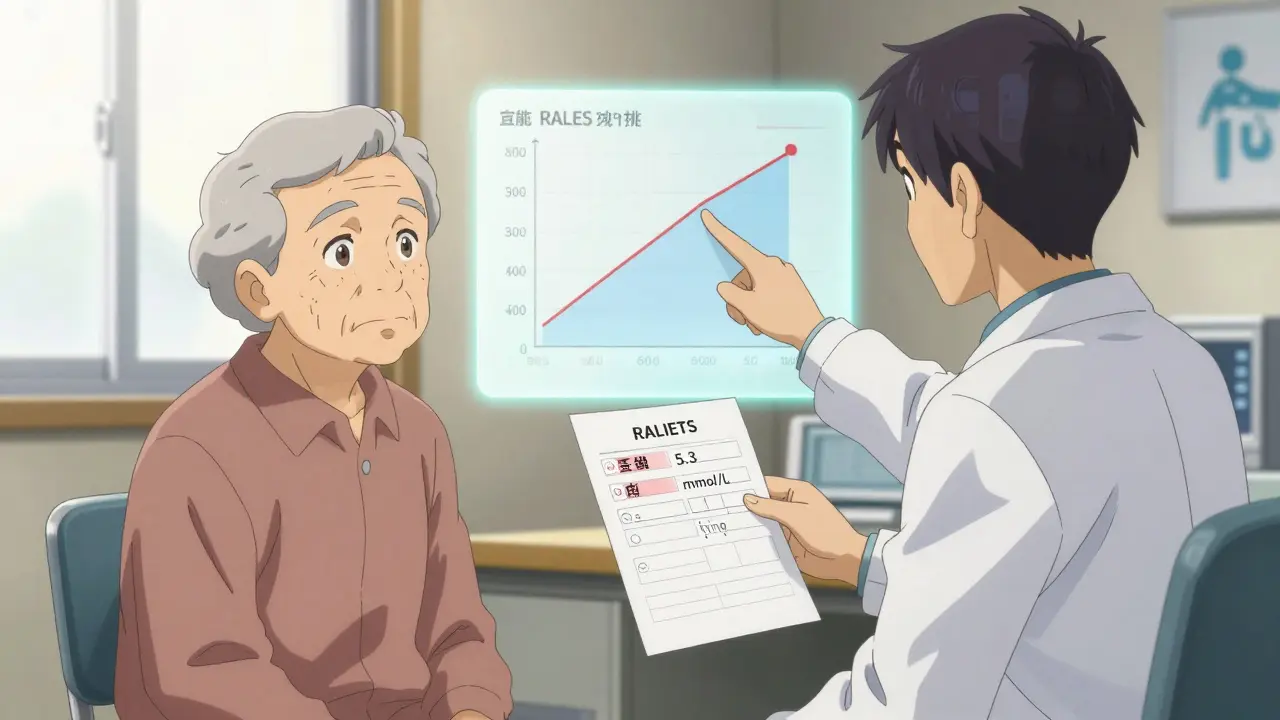
The Evidence: RALES and What It Really Meant
The landmark 1999 RALES trial changed heart failure treatment forever. It showed that adding spironolactone to standard therapy cut death rates by 30% in people with severe heart failure. But it also revealed something troubling: 13.5% of patients on spironolactone developed hyperkalemia (potassium >5.0 mmol/L), compared to just 5% on placebo. And those elevated levels didn’t go away-they stayed high for the entire two-year study. What’s often missed is this: even with higher potassium, patients on spironolactone lived longer. The mortality benefit held up until potassium hit 5.5 mmol/L. That’s critical. It means stopping the drug at 5.1 or 5.2 isn’t always the right move. Many doctors still panic at any rise above 5.0, but the science says: hold off. Don’t quit unless it’s truly dangerous.Who’s Most at Risk?
Not everyone on this combo will get hyperkalemia. But some people are walking into a storm without a raincoat:- People over 70: Age reduces kidney function. A JAMA study found 10% of elderly ACE inhibitor users developed severe hyperkalemia (potassium >6.0 mmol/L) within a year.
- Those with kidney disease: If your creatinine is above 136 µmol/L (1.5 mg/dL) or your eGFR is below 60 mL/min/1.73m², your risk jumps 3.2 times.
- Diabetics: High blood sugar damages kidney blood vessels. That makes potassium harder to clear.
- People already starting with high potassium: If your baseline is over 5.0 mmol/L, you’re already on the edge.
- Those with advanced heart failure: NYHA Class III or IV patients have worse kidney perfusion and fluid overload, which worsens potassium retention.
How to Monitor-And When to Act
Monitoring isn’t optional. It’s the difference between safety and disaster. Here’s what the guidelines say:- Before you start: Check potassium, creatinine, and eGFR. If potassium is already over 5.0, reconsider the combo.
- Within 3-5 days: For high-risk patients (elderly, diabetic, kidney issues), test potassium early. Don’t wait two weeks.
- At 7-14 days: Standard for most patients. If potassium is 5.1-5.5, don’t panic. Adjust the dose instead.
- After every dose change: If you increase spironolactone from 12.5 mg to 25 mg, retest in a week.
- Every 4 months: Even if things look stable, potassium can creep up slowly.
What to Do When Potassium Rises
Don’t automatically stop spironolactone. That’s where many doctors go wrong.- Potassium 5.1-5.5 mmol/L: Reduce spironolactone to 12.5 mg daily. Keep the ACE inhibitor. The mortality benefit still holds at this level.
- Potassium 5.6-6.0 mmol/L: Temporarily stop spironolactone. Recheck in 3-5 days. If potassium drops, restart at a lower dose.
- Potassium >6.0 mmol/L: Stop both drugs immediately. This is a medical emergency. Call 911 if the patient has chest pain, palpitations, or weakness. Treat with calcium gluconate, insulin/glucose, and possibly dialysis.

The Newer Alternatives
Spironolactone isn’t the only option anymore. Finerenone, a newer non-steroidal MRA, was approved after the 2020 FIDELIO-DKD trial showed it caused 6.5% less hyperkalemia than spironolactone in diabetic kidney disease patients. It’s more expensive-$450/month vs. $4/month for generic spironolactone-but for high-risk patients, it’s a game-changer. Another promising angle? Adding SGLT2 inhibitors like empagliflozin. The 2022 EMPA-HEART study found it reduced hyperkalemia events by 22% over 12 months when used with ACE inhibitors and spironolactone. It’s not yet standard, but it’s a sign of where the field is headed: layered protection.Why So Many Patients Still Don’t Get This Treatment
Despite clear survival benefits, only 28.5% of eligible heart failure patients get MRAs like spironolactone. Why? In 63% of cases, doctors cited hyperkalemia fear as the reason. That’s a huge gap between evidence and practice. The 2021 ACC Expert Consensus says it plainly: "The proven mortality benefit of MRAs should not be withheld solely due to mild hyperkalemia." We’re letting fear override science. The key isn’t avoiding the combo-it’s managing it with precision.Bottom Line: Don’t Avoid It. Manage It.
ACE inhibitors and spironolactone together aren’t dangerous because they’re bad-they’re dangerous because they’re powerful. And powerful tools need careful handling. If you’re a patient on this combo:- Know your potassium numbers
- Don’t skip blood tests
- Ask your doctor: "What’s my risk? What’s the plan if it goes up?"
- Don’t stop spironolactone at 5.1
- Start low. Go slow.
- Test early for high-risk patients.
- Consider finerenone or SGLT2 inhibitors for those with repeated hyperkalemia.