Cabergoline vs. Bromocriptine Comparison Tool
Compare Treatment Options
Select the condition you're interested in to see how cabergoline compares to bromocriptine for that specific use case.
When you hear the word cabergoline, you might think of Parkinson’s disease or a rare pituitary tumor, but its role in hormone therapy is expanding fast. In the past decade, doctors have started using this dopamine agonist to treat a host of hormonal imbalances, from excess prolactin to fertility issues. This article breaks down why cabergoline is gaining ground, how it works, who should consider it, and what to watch out for.
Key Takeaways
- Cabergoline is a long‑acting dopamine agonist that lowers prolactin levels more effectively than older drugs.
- It’s now a first‑line option for prolactinoma, hyperprolactinemia‑related infertility, and even off‑label hormone‑balancing protocols.
- Compared with bromocriptine, cabergoline offers fewer side effects, a simpler dosing schedule, and better patient adherence.
- Regular monitoring of heart valves and blood pressure is essential, especially for high‑dose or long‑term use.
- Emerging research suggests potential uses in estrogen‑dominant conditions and metabolic health, but more trials are needed.
What Is Cabergoline?
Cabergoline is a synthetic ergoline derivative that functions as a potent dopamine D2‑receptor agonist. First approved in the early 1990s for Parkinson’s disease, it quickly found a niche in endocrinology because stimulating dopamine receptors suppresses prolactin secretion from the pituitary gland. Lowering prolactin helps shrink prolactin‑secreting tumors (prolactinomas) and restores normal reproductive hormones.
How Cabergoline Works in Hormone Therapy
Prolactin is a hormone produced by the anterior pituitary that mainly drives milk production after childbirth. When prolactin levels stay high for other reasons-stress, certain medications, or a tumor-the hormone can interfere with the hypothalamic‑pituitary‑gonadal (HPG) axis. High prolactin suppresses the release of gonadotropin‑releasing hormone (GnRH), which in turn reduces luteinizing hormone (LH) and follicle‑stimulating hormone (FSH). The result? Irregular periods, infertility, low testosterone in men, and sometimes galactorrhea (unexpected milk discharge).
By binding to dopamine D2 receptors on lactotroph cells, cabergoline mimics the brain’s natural dopamine brake on prolactin. The drug’s long half‑life (about 65 hours) means it can be taken just once or twice a week, providing steady suppression without the peaks and troughs that older agents produce.
Primary Clinical Uses in Hormone Therapy
While cabergoline still carries a Parkinson’s label, clinicians now prescribe it for several hormone‑related conditions:
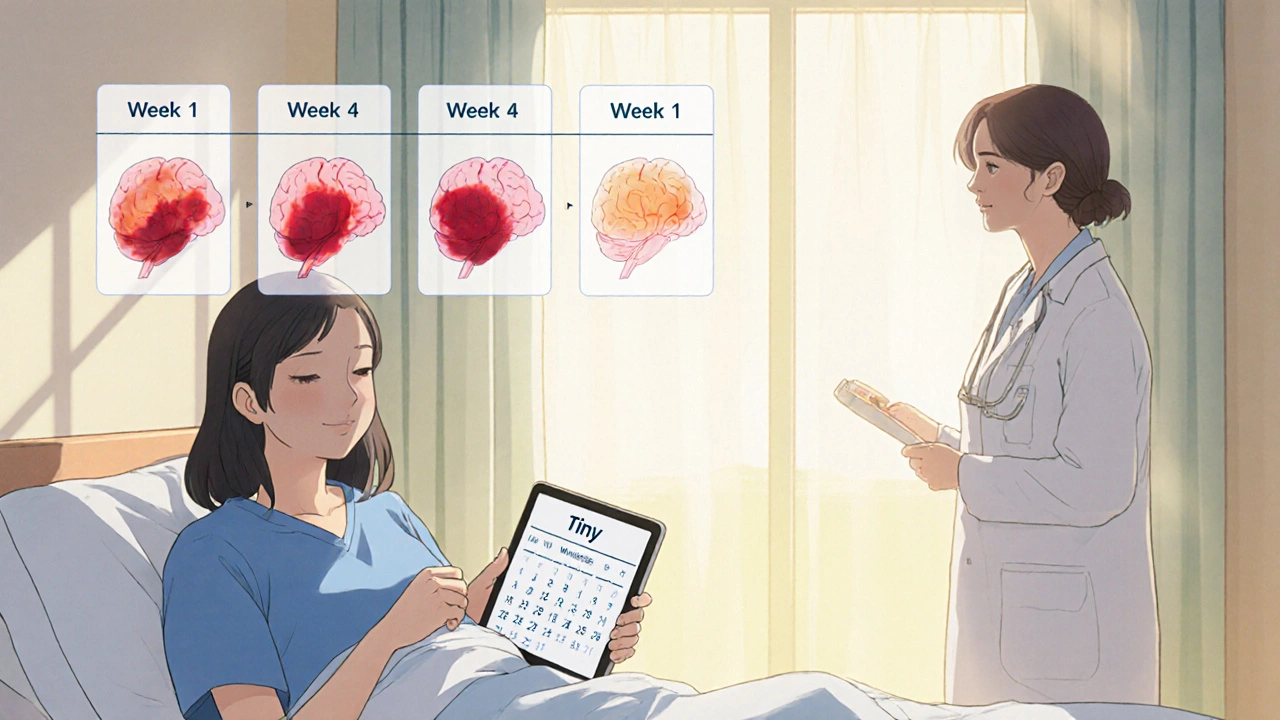
- Prolactinoma: The drug shrinks tumors in 80‑90% of patients and normalizes prolactin in most cases.
- Hyperprolactinemia‑related infertility: Women with unexplained anovulation often see their cycles return within weeks of treatment.
- Male hypogonadism linked to high prolactin: Restores testosterone levels and improves libido.
- Off‑label estrogen‑dominant disorders: Some specialists use low‑dose cabergoline to lower estradiol in polycystic ovary syndrome (PCOS) or uterine fibroids, though evidence is still emerging.
Comparing Cabergoline to Other Dopamine Agonists
| Attribute | Cabergoline | Bromocriptine |
|---|---|---|
| Typical Dose for Prolactinoma | 0.5‑1 mg once weekly | 2.5‑5 mg daily |
| Half‑Life | ≈65 hours | ≈12 hours |
| Prolactin Normalization Rate | ~85‑90% | ~65‑70% |
| Most Common Side Effects | Nausea, dizziness, mild hypotension | Nausea, constipation, headache |
| Risk of Valvular Heart Disease | Low at standard doses; higher risk only >3 mg/week long‑term | Rare |
The table shows why many endocrinologists prefer cabergoline: fewer pills, better adherence, and a higher chance of tumor shrinkage. However, the longer half‑life also means that any side effect can linger, so doctors monitor patients closely during the first few weeks.
Benefits of Cabergoline in Hormone Therapy
- Convenient dosing: Once‑or‑twice‑weekly tablets simplify life for busy patients.
- High efficacy: Rapid prolactin reduction often translates into quicker menstrual regularity or tumor shrinkage.
- Fewer gastrointestinal complaints compared with bromocriptine, making it easier to stay on therapy.
- Potential metabolic perks: Early studies suggest modest improvements in insulin sensitivity for women with PCOS, though more research is needed.
Risks and What to Watch For
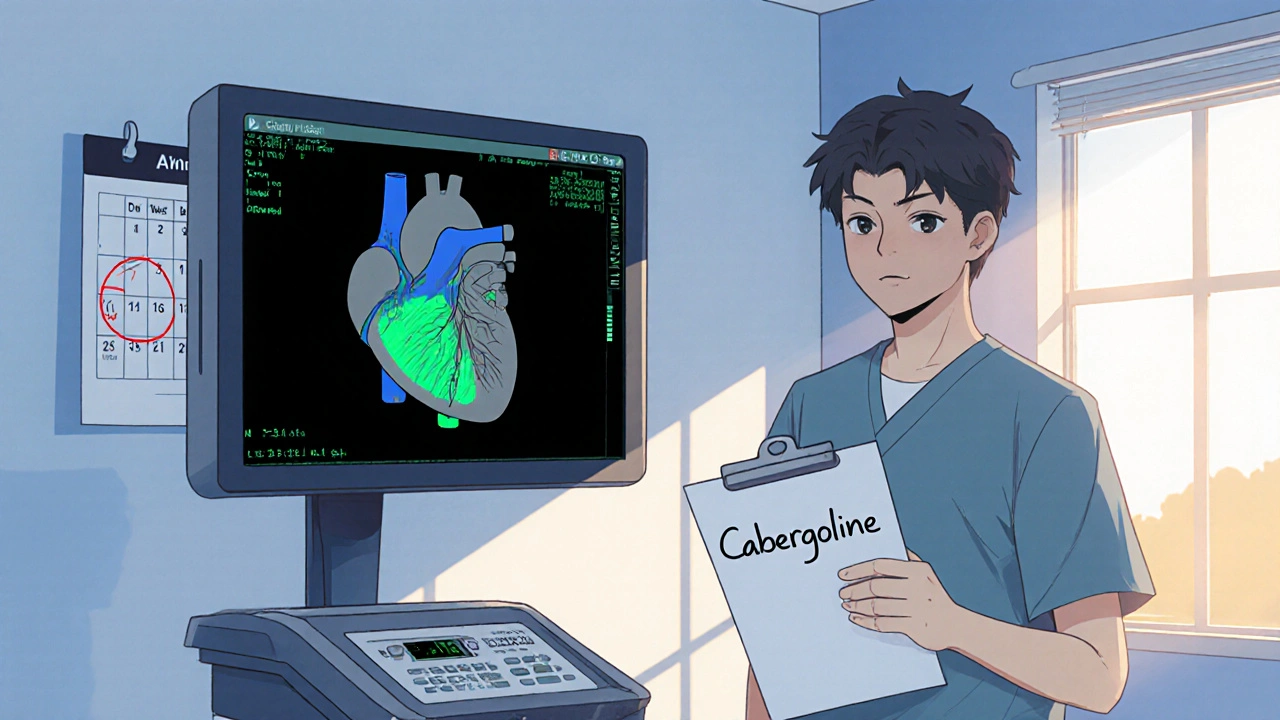
Every medication has downsides, and cabergoline is no exception. The most discussed safety issue is valve‑related heart disease, a concern that emerged from high‑dose Parkinson’s studies. In hormone‑therapy doses (<1 mg/week), the risk is low, but clinicians still order an echocardiogram at baseline and then annually if treatment exceeds two years.
Other side effects include:
- Nausea or stomach upset (usually resolves within a few days).
- Dizziness or light‑headedness, especially when standing quickly.
- Rare psychiatric effects such as vivid dreams or mood swings.
If any symptom persists, the doctor may adjust the dose or switch to an alternative.
Practical Tips for Patients Starting Cabergoline
- Take with food to reduce nausea.
- Stay hydrated and avoid sudden changes in posture to prevent dizziness.
- Track symptoms in a journal-note menstrual changes, headaches, or any new chest discomfort.
- Schedule regular labs: Prolactin, liver enzymes, and a baseline echocardiogram.
- Communicate with your provider about any other meds you’re on. Some antipsychotics and anti‑emetics can interfere with dopamine pathways.
The Future Landscape: Ongoing Research and Emerging Uses
Researchers are exploring cabergoline beyond classic prolactin‑related disorders. Trials are investigating low‑dose regimens for:
- Men with low testosterone linked to high prolactin.
- Women with PCOS who don’t respond to first‑line lifestyle changes.
- Patients with metabolic syndrome, looking at insulin‑sensitivity improvements.
While results are promising, regulatory bodies still await large‑scale data before updating official labeling. For now, the drug’s main strength remains its proven track record in prolactinoma and hyperprolactinemia.
Bottom Line
Cabergoline has reshaped hormone therapy by offering a potent, once‑weekly option that outperforms older dopamine agonists in most respects. For anyone dealing with excess prolactin, the medication can restore hormonal balance, spare invasive surgery, and improve quality of life. As long as patients keep up with monitoring and stay alert to side effects, cabergoline is likely to stay a mainstay in endocrinology for years to come.
Can cabergoline be used for weight loss?
There is no strong evidence that cabergoline directly causes weight loss. Some patients notice a modest reduction in appetite, but it’s not approved for this purpose. Weight changes are usually a side effect of improved hormone balance rather than a primary benefit.
How long does it take for prolactin levels to normalize?
Most patients see a drop within 2‑4 weeks of starting therapy, with full normalization often occurring by 3‑6 months, depending on tumor size and dose.
Is cabergoline safe during pregnancy?
Cabergoline is generally discontinued once pregnancy is confirmed because dopamine agonists can affect fetal development. Your doctor will guide you on when to stop and what alternative monitoring is needed.
What should I do if I miss a dose?
Take the missed tablet as soon as you remember, unless it’s been more than 24 hours. In that case, skip the missed dose and resume your regular weekly schedule. Don’t double‑dose.
Do I need regular heart scans while on cabergoline?
A baseline echocardiogram is recommended before starting high‑dose therapy. For standard hormone‑therapy doses (<1 mg/week), an annual scan is usually sufficient, but your doctor may adjust the frequency based on your health history.

Vandermolen Willis
October 22, 2025 AT 16:23Cabergoline really changed the game for folks dealing with high prolactin 😊. The once‑daily dosing of older drugs can be a hassle, but taking a tablet once a week now makes life smoother. Most patients I’ve seen report fewer nausea episodes and better adherence. It’s still vital to get those echo checks every now and then, especially if you’re on higher doses. Overall, it’s a solid option that many endocrinologists are leaning toward.
Mary Keenan
October 31, 2025 AT 21:37Honestly, the hype around cabergoline is overblown – the side‑effects are still a gamble.
cariletta jones
November 10, 2025 AT 03:50For anyone juggling fertility issues, cabergoline offers a quick route back to regular cycles – a bright spot in hormone therapy.
Kevin Hylant
November 19, 2025 AT 10:03Cabergoline works because it hits dopamine receptors hard, slashing prolactin fast. It’s not a miracle pill, but it’s far better than the old bromocriptine regimen.
Holly Green
November 28, 2025 AT 16:17We should stop glorifying drugs without demanding full transparency on long‑term cardiac risks.
Craig E
December 7, 2025 AT 22:30While the pharmacological virtues of cabergoline are undeniable, one must also contemplate the ethical dimension of prescribing a medication with a known, albeit rare, propensity for valvular heart disease. The clinician’s duty, therefore, extends beyond mere biochemical correction; it embraces vigilant surveillance and informed consent, ensuring patients are not merely subjects of biochemical manipulation but partners in their therapeutic journey.
Marrisa Moccasin
December 17, 2025 AT 04:43Did you know-just in case you missed it-that pharmaceutical companies have been pushing cabergoline as a “miracle” while quietly ignoring the mounting data on valve abnormalities??? It’s all part of a larger agenda to monetize every hormonal imbalance!
Caleb Clark
December 26, 2025 AT 10:57If you're feeling lost in the maze of hormone treatments, remember that cabergoline can be a steady lighthouse guiding you toward balance.
First off, the dosing schedule-just one or two pills a week-means you don't have to juggle a dozen reminders each day.
That simplicity alone can lift a huge mental load, letting you focus on what matters, like getting back to the gym or spending time with family.
Clinical studies show that prolactin levels drop dramatically within weeks, often restoring regular menstrual cycles for many women.
Men on the drug report a noticeable boost in testosterone and libido, which can reignite confidence that was dulled by chronic fatigue.
Of course, no medication is without a shadow, so never skip the cardiac echo after a few months of therapy.
Your doctor will watch for any valve changes, and most patients never see any issues, but vigilance is key.
Another perk is the reduced nausea compared to bromocriptine-most folks say they can finally enjoy a hearty breakfast without queasy feelings.
Plus, there are hints that cabergoline might improve insulin sensitivity, a bonus for anyone battling PCOS or metabolic syndrome.
Stay consistent with your appointments, because the half‑life of the drug means it stays in your system for days, smoothing out peaks and troughs.
Never underestimate the power of community support; sharing your experience on forums can provide encouragement and practical tips.
Set a small goal each week-like tracking your cycle or noting energy levels-and celebrate those wins, no matter how tiny.
Remember, you’re not alone in this journey; countless peers have walked the path and emerged stronger.
If side effects creep in, talk to your physician promptly; dose adjustments are often enough to keep you on track.
Above all, keep faith in the process, stay proactive, and trust that with the right guidance, cabergoline can be a game‑changer in reclaiming your health.
Eileen Peck
January 4, 2026 AT 17:10One practical tip: schedule a baseline echocardiogram before starting cabergoline, then repeat it annually if you’re on a higher dose. This helps catch any valve changes early, keeping your heart health in check.