Every morning, hundreds of thousands of children across the U.S. take their prescribed medications at school. Some need insulin for diabetes. Others rely on inhalers for asthma or stimulants for ADHD. For many, school is where their treatment plan becomes real - and where a single mistake can have serious consequences. That’s why coordinating school nurses for daily pediatric medications isn’t just a task - it’s a system that must work flawlessly, every single day.
Why School Nurses Are the Key to Safe Medication Delivery
School nurses aren’t just the first responders when a kid falls off the monkey bars. They’re the central hub for managing complex medical needs during school hours. With over 14.7% of students requiring daily medications - and 92% of school districts having formal policies - the role of the school nurse has shifted from reactive care to proactive coordination. The five rights of medication administration - right student, right medication, right dose, right route, right time - are the foundation. But in schools, these aren’t just nursing principles. They’re legal requirements backed by the National Association of School Nurses (NASN) 2022 Clinical Practice Guideline and reinforced by the American Academy of Pediatrics (AAP) in 2024. Missing one right isn’t an oversight; it’s a risk that can lead to liability, regulatory action, or worse.Step 1: Build a District-Wide Medication Policy
You can’t manage what you don’t document. Every district needs a clear, written policy that answers: Who can give meds? What forms are required? Where are they stored? How are errors reported? Start with NASN’s sample policy templates. These aren’t suggestions - they’re the gold standard. A strong policy includes:- Requirements for original, pharmacy-labeled containers (21 CFR § 1306.22)
- Procedures for controlled substances (double-counting, dual signatures)
- Clear delegation rules for unlicensed personnel
- Emergency protocols for epinephrine, glucagon, or seizure meds
Step 2: Screen Students and Create Individualized Healthcare Plans (IHPs)
Not all students need the same level of support. Use a three-tier system like New York’s:- Nurse Dependent: Students who need full nursing care (e.g., IV medications, complex insulin regimens)
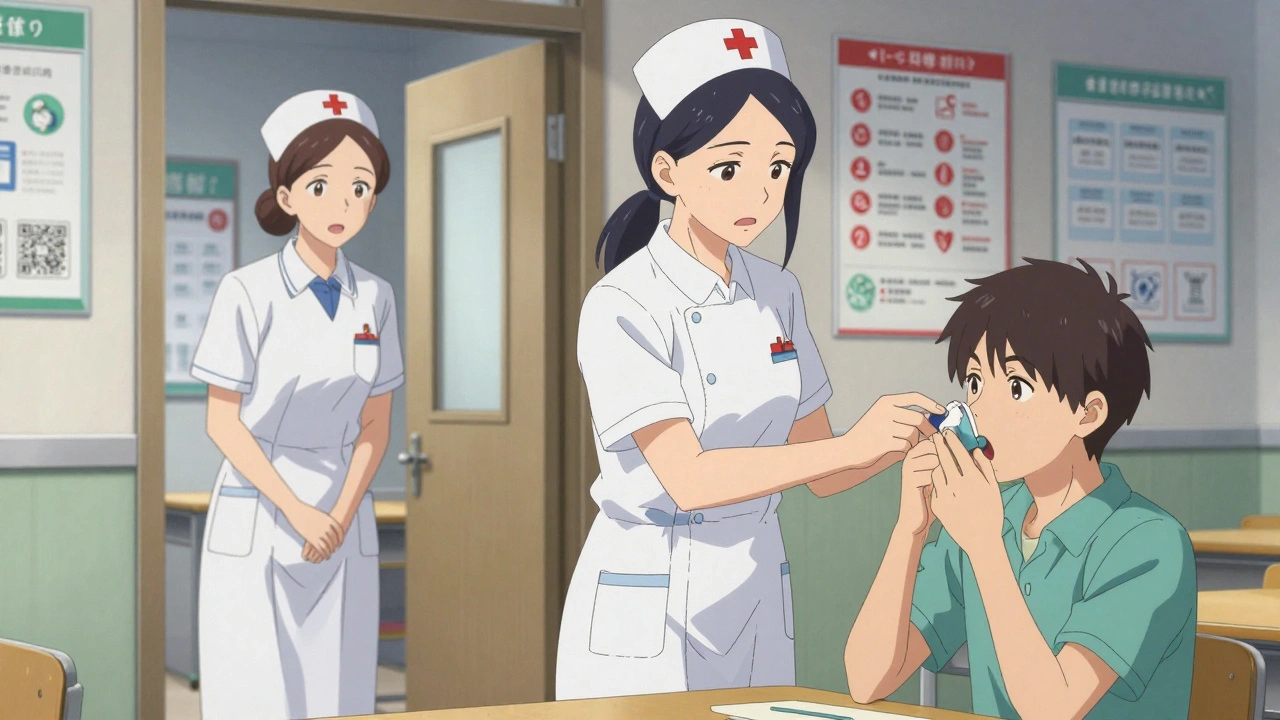
- Supervised: Students who can self-administer but need oversight (e.g., asthma inhalers)
- Self-Administered: Students with permission to carry and use their own meds (e.g., epinephrine auto-injectors)
- Medication schedule
- Side effects to watch for
- Emergency contacts
- Parent and provider signatures
Step 3: Train the Right People - and Only the Right People
School nurses can’t be everywhere. That’s why delegation is necessary. But delegation isn’t handing off a pill bottle. Before assigning a task to a teacher, aide, or bus driver, the nurse must:- Assess the student’s medical complexity
- Assess the staff member’s competence
- Provide training (4-16 hours, depending on the med)
- Document competency
- The five rights
- How to read pharmacy labels
- What to do if the student vomits or refuses the med
- When to call the nurse
Step 4: Choose and Use the Right Documentation System
Documentation isn’t busywork. It’s your legal shield. As of 2023, 98% of districts use electronic health records (EHRs) for medication logs. But 42 states still allow paper logs. Paper is cheaper. But it’s also slower, error-prone, and harder to audit. Fairfax County Public Schools switched to an EHR system and cut documentation time by 45%. Accuracy jumped 31%. The system auto-flags missed doses, reminds staff when meds are due, and syncs with parent portals. If you’re stuck with paper:- Use pre-printed, tamper-proof logs
- Require initials and time stamps for every dose
- Store logs in locked cabinets
- Review them daily
Step 5: Handle Emergency Medications Like Clockwork
Anaphylaxis, seizures, severe hypoglycemia - these don’t wait for the nurse to finish grading papers. Every school should have:- Stock epinephrine (87% of U.S. schools do)
- Glucagon for diabetes emergencies
- Seizure rescue meds (like midazolam)
- Trained staff must know where the kits are
- They must be checked monthly for expiration
- They must be restocked immediately after use
Step 6: Build a Just Culture for Error Reporting
Mistakes happen. The goal isn’t to eliminate them - it’s to learn from them. A “Just Culture” framework treats errors as system failures, not personal failures. In pilot districts, this approach reduced medication errors by 37% in one year. How it works:- Report errors anonymously
- Review them monthly in team meetings
- Ask: What broke? Not: Who messed up?
Step 7: Review, Improve, and Advocate
Medication coordination isn’t a one-time project. It’s a cycle. Monthly, review:- Missed doses
- Parent non-compliance (38% of districts report parents bring meds in plastic bags)
- Staff turnover
- Changes in student health needs

What Parents Need to Know - And How to Help Them
Parents are partners. But they’re often confused. Many bring meds in ziplock bags. Others forget to update dosage changes. Some think a doctor’s note replaces a pharmacy label. Host mandatory parent education sessions. Show them:- What a proper pharmacy label looks like
- Why they can’t bring meds from home in unlabeled containers
- How to update the IHP when prescriptions change
Common Pitfalls and How to Avoid Them
- Pitfall: Using expired meds. Solution: Monthly inventory checks.
- Pitfall: Letting untrained staff give insulin. Solution: Only RNs or trained personnel under direct supervision.
- Pitfall: Assuming a student’s med plan hasn’t changed. Solution: Reassess IHPs every semester.
- Pitfall: Ignoring field trips and after-school activities. Solution: Extend protocols to all school-sponsored events.
Resources You Can’t Afford to Ignore
- NASN Implementation Toolkit: Free templates for policies, training, and IHPs. 89% of nurses say it’s “extremely valuable.”
- CDC School Health Guidelines: Evidence-based standards for all school health services.
- State School Nurse Association: Connect with peers. Ask questions. Share solutions.
- NASN 24/7 Consultation Line: Used by 63% of members. Call when you’re unsure.
What’s Next? Technology and the Future
By 2026, 63% of districts will pilot smartphone-based systems that let staff scan a QR code on a medication bottle to verify the right student, right dose, right time - before giving it. Telehealth integration is also coming. Nurses will be able to video-call parents or prescribers during school hours to clarify orders. But no tech replaces good judgment. No app can tell you if a child looks pale, shaky, or confused. That’s why the school nurse remains irreplaceable.Coordinating daily pediatric medications in school is hard. It’s messy. It’s exhausting. But it’s also vital. Every child deserves to be safe, healthy, and ready to learn - no matter their medical needs. The system works when nurses lead it, staff follow it, parents support it, and districts fund it.
Can a teacher give a child their medication?
Yes - but only if the school nurse has assessed the child’s needs, trained the teacher, documented competency, and the medication is low-risk (like an inhaler or antihistamine). For complex meds like insulin or seizure rescue drugs, only licensed nurses or staff under direct RN supervision can administer them.
What if a parent brings medication in a plastic bag?
Do not accept it. Federal law (21 CFR § 1306.22) requires all medications in schools to be in original, properly labeled pharmacy containers. If a parent brings meds in a plastic bag, explain the law, offer to help them get a new prescription filled, and provide a temporary supply from school stock if available and authorized.
Do I need a doctor’s note for every medication?
Yes - but a doctor’s note is not enough. You also need the original pharmacy-labeled container, a completed Individualized Healthcare Plan (IHP), and parent consent. The note confirms the need; the label confirms the identity and dosage.
How often should medication logs be reviewed?
Daily. The school nurse or designated staff should review all medication logs at the end of each school day to catch missed doses, errors, or inconsistencies. Monthly audits by the district’s health coordinator are required for compliance.
What happens if a school doesn’t follow medication protocols?
Non-compliance can lead to serious consequences: federal funding loss (as seen in Houston ISD’s $2.3 million sanction), state health department citations, lawsuits from families, and loss of accreditation. More importantly, it puts children at risk of harm or death.
Is there a shortage of school nurses?
Yes. The national average is 1 nurse for every 1,102 students. Experts recommend 1:750 for schools with complex medical needs. By 2027, a 15% nursing shortage is projected. This forces districts to rely on unlicensed staff, increasing risk. Advocacy and funding are critical to fix this.


patrick sui
December 1, 2025 AT 14:21Let’s be real - the five rights are the bare minimum. But what about the *sixth right*? Right context. A kid with asthma might be fine in class but panic during PE. Nurses need to assess not just the med, but the environment. I’ve seen kids denied inhalers because ‘it’s not on the schedule’ - but their triggers aren’t clockwork. 🤦♂️
Conor Forde
December 3, 2025 AT 04:17So… we’re now treating school nurses like pharmacists + cops + therapists + HR? And the district won’t even pay for a damn EHR? 😭 I swear if one more parent shows up with a Ziploc full of Ritalin, I’m starting a petition to turn the nurse’s office into a bunker with armed guards. #MedicationMadness
Declan O Reilly
December 4, 2025 AT 11:27There’s a quiet revolution happening here. We’re not just managing pills - we’re managing trust. When a kid knows their insulin won’t be forgotten, or their EpiPen is always within reach, they stop fearing school. That’s not policy. That’s humanity. And it’s not expensive - it’s essential. The real cost? Not having enough nurses to hold that space. 🌱
Declan Flynn Fitness
December 5, 2025 AT 19:00Biggest win I’ve seen? When schools let kids carry their own inhalers. No paperwork. No delays. Just freedom. Kids feel respected. Nurses get to focus on the complex cases. Win-win. Just make sure they know how to use it. 😎
soorya Raju
December 7, 2025 AT 14:32Whoa. Hold up. So now the feds are telling us how to give kids their meds? Next they’ll be scanning our kids’ blood for ‘compliance data’. This is the slippery slope to the NWO health surveillance state. I’ve seen kids given meds they don’t need - ADHD pills for ‘disruptive behavior’. It’s chemical control. 🚩
Dennis Jesuyon Balogun
December 8, 2025 AT 21:55Let me tell you something - this isn’t about policy. It’s about power. The system wants control. The nurse becomes the gatekeeper. The parent becomes the liability. The child becomes a case file. And the real question? Who benefits when we make healthcare so bureaucratic that only the privileged can navigate it? This isn’t safety - it’s institutionalized exclusion. 🔥
Grant Hurley
December 10, 2025 AT 02:47Just had a mom drop off her kid’s meds in a Starbucks cup. I told her ‘nope’ - she cried. So I called the pharmacy, got a new bottle delivered by noon, and gave her a hug. We’re not robots. Sometimes the system fails - but we don’t have to. 😊
Lucinda Bresnehan
December 11, 2025 AT 07:26One thing nobody talks about: the emotional labor. I had a 9-year-old with type 1 diabetes who would cry every morning because she was scared of the needle. I sat with her for 20 minutes every day for three weeks. No meds were given until she felt safe. That’s nursing. Not policy. Not protocol. Just presence. 🫂
Shannon Gabrielle
December 13, 2025 AT 05:49Wow. A 7-step guide to make nurses into corporate compliance robots. And we wonder why they quit? 🙄 Next they’ll require a background check to hand out Tylenol. At this point, why not just strap kids to IV poles and call it ‘healthcare efficiency’?
ANN JACOBS
December 14, 2025 AT 11:51It is imperative, and indeed, of the utmost moral and ethical significance, that we recognize the profound, transcendent responsibility entrusted to school nursing personnel - not merely as functionaries of pharmacological administration, but as custodians of the sacred trust between the family, the institution, and the vulnerable child. The sanctity of the medication protocol is not a bureaucratic formality - it is the very fabric of societal integrity. Failure to uphold this standard is not negligence - it is a moral breach of the highest order. We must act, not with haste, but with reverence.
Nnaemeka Kingsley
December 14, 2025 AT 18:14My cousin in Lagos, Nigeria - his kid got asthma at school. No nurse. No meds. Just a teacher who knew how to use the inhaler. They learned from YouTube. Sometimes, you don’t need a policy. You just need someone who cares. 🙏
Kshitij Shah
December 16, 2025 AT 00:03Y’all really think this works? In India, we have 1 nurse for 5,000 kids. We use sticky notes on the fridge. And guess what? Kids still get their meds. Maybe the problem isn’t the system - it’s that we over-engineer everything. Just train the teachers. Let the parents help. Stop making it a federal case. 🤷♂️