Every time you pick up a prescription, there’s a simple step that could keep you safe: confirming your name and medication on the prescription label. It takes less than 30 seconds. But skipping it can lead to serious mistakes - like taking the wrong drug, the wrong dose, or someone else’s medicine. You might think the pharmacy got it right. But errors happen more often than you’d expect.
Why This Step Matters
About 1.5 million people in the U.S. are affected by medication errors every year. Nearly a quarter of those are caused by wrong labels. That’s not because pharmacists are careless. It’s because mistakes can slip in at any point - a mix-up in the back, a misread handwriting, a computer glitch, or even two patients with similar names getting their bottles swapped. The label is your last line of defense. Before you walk out the door, you need to check it yourself.A 2020 study in the Journal of the American Pharmacists Association found that patients who verified their labels reduced their risk of taking the wrong medication by 67%. That’s not a small number. It’s life-changing.
What to Look For on the Label
Every legal prescription label in the U.S. must include six key pieces of information. Don’t just glance - read them out loud if you can. Here’s what to check:- Your full legal name - First, middle, and last. Not “Wyn” if your ID says “Wyn Davies.” Not “J. Smith” if your name is “Jennifer Smith.”
- The medication name - Both the brand name (like “Lipitor”) and the generic name (like “atorvastatin”) should be listed. If your doctor told you “the cholesterol pill,” make sure the label matches what you were told.
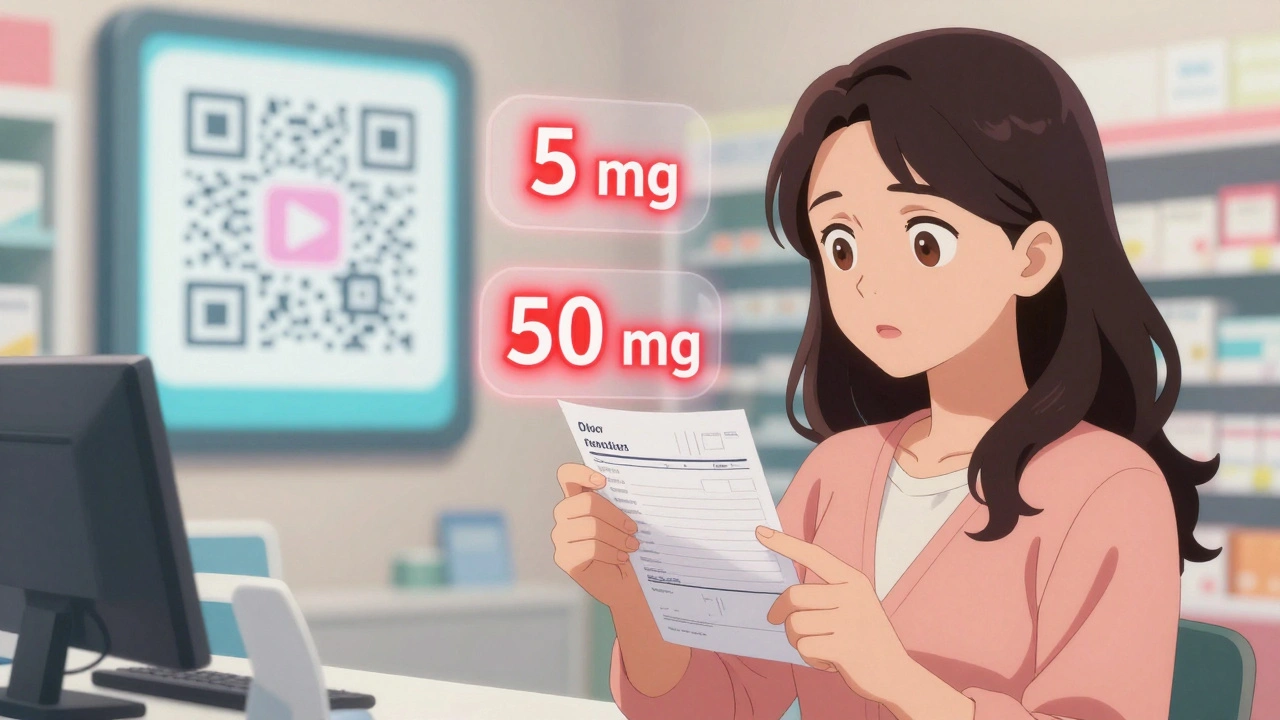
- The strength - This is where mistakes are most common. “5 mg” is not the same as “50 mg.” If your doctor said “5 mg once a day,” but the label says “10 mg,” stop. Ask.
- The directions - “Take one tablet by mouth twice daily” should match what your doctor explained. If it says “every 6 hours” and you were told “every 12 hours,” something’s off.
- The pharmacy name and phone number - It should be the pharmacy you picked it up from. If it’s a different one, that’s a red flag.
- The prescription number and date - These help the pharmacy track your record. If the date is from last month and you just got the script today, double-check.
The FDA recommends you verify these five things every time: your name, the drug name, the strength, the directions, and the pharmacy contact info. Don’t leave out the strength - it’s the most common error.
Common Mistakes People Miss
Many patients think, “My name is on it, so it must be mine.” But that’s not enough. Here are real examples of what goes wrong:- A woman picked up her blood thinner and saw her name. The pill looked different - but she didn’t check the strength. It was 10 mg instead of 5 mg. She almost took a dangerous overdose.
- A man grabbed his wife’s prescription because her name was on the bottle. He had the same first name and similar last name. The pharmacist mixed them up.
- An elderly patient took a diabetes pill because the label had his name. But the drug was for high blood pressure. He didn’t know the generic name and didn’t ask.
According to a 2023 survey by the National Patient Safety Foundation, 18% of people found an error on their label in the past year. Most of those errors were caught because they checked.
What to Do If Something Looks Wrong
Don’t guess. Don’t assume. Don’t take it home and hope it’s fine.Go back to the pharmacist. Say: “I’m checking my prescription. The label says [medication name], but my doctor prescribed [different name]. Can you confirm this is right?”
Pharmacists are trained to help with this. They’ve seen it before. They won’t think you’re being difficult - they’ll be glad you asked. In fact, the American Medical Association says doctors should expect patients to check. They even recommend telling patients to do it.
If the pharmacist says, “It’s correct,” ask to see the original prescription from your doctor. Most pharmacies can pull it up on screen. Compare it side by side. If you’re still unsure, call your doctor’s office. Keep the bottle with you - don’t leave it behind.
Helpful Tools for Easier Verification
If you have trouble reading small print, you’re not alone. Nearly 40% of people over 65 struggle with it. Here’s how to make it easier:- Use a pocket magnifier - they cost less than $10 and fit in your wallet.
- Turn on your phone’s magnifier app. Most smartphones have one built in. Just open the camera, pinch to zoom, and hold it over the label.
- Ask for a large-print label. Many pharmacies - especially CVS and Walgreens - offer this if you ask. Some even print it on a separate card.
- Use a flashlight. Poor lighting makes small text harder to read. Hold the bottle under a bright light.
- Bring a list. Write down your medications and doses before you go. Hold it next to the label while you check.
Some pharmacies now have verification stations with magnifiers and lighting built in. Ask if they have one. About 78% of CVS locations and 65% of Walgreens do.
Why Digital Apps Aren’t Enough
Apps like Medisafe or GoodRx let you scan your label and track doses. That’s useful. But they’re not replacements for checking the physical label.Why? Because:
- Not everyone has a smartphone - especially older adults.
- Apps can’t catch a label that was printed wrong in the first place.
- If you’re in a hurry, you won’t open the app. But you can look at the bottle.
Think of apps as helpers - not safety nets. The real safety net is you, looking at the bottle before you leave the pharmacy.
What’s Changing Soon
By the end of 2025, the FDA will require all prescription labels in the U.S. to follow a new standard. The biggest change? Your name will be printed in 24-point font at the very top. That’s huge. Right now, it’s often buried in small text. This new rule is meant to make it impossible to miss.Also, more pharmacies will start putting QR codes on labels that link to short videos explaining your medication in your language. By 2026, 60% of prescriptions for people over 65 are expected to include them. That’s a big step toward making safety easier for everyone.
Final Checklist Before You Walk Out
Use this quick 30-second routine every time:- Hold the bottle at eye level under good light.
- Find your full name - is it spelled exactly right?
- Find the medication name - does it match what your doctor said?
- Check the strength - is it 5 mg, not 50 mg?
- Read the directions - does it say “once daily” or “twice daily”?
- Confirm the pharmacy name and number are correct.
If all six match - great. You’re safe. If even one doesn’t - stop. Ask.
What If You’re Helping Someone Else?
If you’re picking up meds for a parent, spouse, or friend, treat it like your own. Don’t assume they can check it themselves. Older adults, people with vision problems, or those with memory issues rely on you. Make the check part of your routine. Write down what you see. Call the pharmacy if anything seems off. You’re not overstepping - you’re saving a life.What if my name is misspelled on the prescription label?
Don’t take the medication. Even a small spelling error - like “Wyn” instead of “Wynne” - can mean it’s not your prescription. Go back to the pharmacy immediately. They can correct it and reprint the label. Never assume it’s a typo - it could be someone else’s medicine.
Can I trust the pharmacy to get it right without checking?
No. Even the best pharmacies make mistakes. Pharmacists are human, systems can glitch, and similar-looking drugs can be mixed up. The label is your final safety check. Relying only on the pharmacy increases your risk. Checking your label is the most effective way to prevent a medication error.
What should I do if I can’t read the label?
Don’t guess. Ask the pharmacist to read it to you out loud. Most pharmacies have magnifiers or large-print labels available. You can also use your phone’s camera zoom feature to enlarge the text. If you’re still unsure, call your doctor’s office and have them confirm the details. Your safety is worth the extra step.
Why does the label sometimes show a different name than what my doctor prescribed?
That’s usually the generic version. For example, your doctor may say “Lipitor,” but the label says “atorvastatin.” Both are the same drug. Ask the pharmacist if you’re unsure. They can explain the difference. Never assume it’s a mistake unless the drug type is completely different.
Is it normal for the strength to change between refills?
Only if your doctor changed it. If you’ve been on 5 mg for months and suddenly get 10 mg, that’s not normal. Call your doctor’s office before taking it. Strength changes can be dangerous, especially with blood thinners, diabetes meds, or heart medications. Always verify.
What if I don’t have time to check at the pharmacy?
Take the time. Even if you’re in a rush, don’t skip this step. You can always put the bottle in your bag and check it in the car. But never take the medication without confirming the label matches what you were prescribed. A few extra minutes can prevent an emergency room visit.
Can I get a printed copy of my prescription to compare?
Yes. Most pharmacies can print a copy of the original prescription from your doctor. Just ask. Keep it with you - it’s your best tool for verifying that the label matches what was ordered. Some doctors also send digital copies through patient portals - check those too.
Next Steps for Better Safety
Start today. The next time you pick up a prescription, pause. Don’t rush. Read the label like your life depends on it - because it does. Make it a habit. Tell your family to do the same. If you help someone else, make it part of your routine. And if you ever feel unsure - ask. Pharmacists are there to help. You’re not bothering them. You’re doing exactly what they want you to do.By 2027, experts estimate that if everyone checked their labels, we could prevent 300,000 dangerous drug events each year. That’s not a guess. That’s based on data from the Agency for Healthcare Research and Quality. You’re not just protecting yourself - you’re part of a bigger safety system.


Karandeep Singh
December 2, 2025 AT 18:34lol pharmacy errors? bro in india we just grab the bottle and go. if u get the wrong pill u die. simple. no labels needed. my grandma takes 12 meds and never checked once. still alive. lol
Alexander Williams
December 2, 2025 AT 22:35The foundational flaw in this narrative is the implicit assumption that label verification is a sufficient risk mitigation strategy in a system with systemic pharmacovigilance failures. The burden of cognitive load is externalized onto the patient-this is a classic case of institutional liability displacement. The real issue lies in the lack of standardized barcoding interoperability between EHRs and dispensing systems, not patient diligence.
Suzanne Mollaneda Padin
December 4, 2025 AT 19:25I work at a community pharmacy and I can tell you-patients who check their labels are the ones we love the most. We don't mind the extra minute. In fact, we often say, 'Go ahead, read it out loud, I'll wait.' It gives us a chance to catch our own mistakes too. And yes, we do have large-print labels. Just ask. No shame in needing help reading small text. We've all been there.
Amber-Lynn Quinata
December 5, 2025 AT 03:57I just found out my neighbor took someone else's blood thinner because she didn't check the name. She almost died. 😭 I told her she should've known better. How can you be so careless? You're not just risking your life-you're risking everyone's peace of mind. 🙄
Lauryn Smith
December 5, 2025 AT 16:38This is such a simple thing to do but so many people skip it. I used to rush out of the pharmacy too-until my mom had a bad reaction because the dose was wrong. Now I check every time. I even bring a pen and paper to write down what I see. It takes 30 seconds. That's less time than scrolling through Instagram. Your life is worth it.
Bonnie Youn
December 7, 2025 AT 01:52STOP WASTING TIME WITH THIS BASIC STUFF IF YOU'RE NOT CHECKING YOUR LABELS YOU DESERVE WHAT YOU GET I'M NOT KIDDING I'VE SEEN PEOPLE END UP IN THE ER OVER THIS AND IT'S 100% AVOIDABLE JUST LOOK AT THE BOTTLE BEFORE YOU LEAVE YOU'RE NOT TOO BUSY FOR YOUR OWN LIFE
elizabeth muzichuk
December 8, 2025 AT 06:14This is all part of the pharmaceutical-industrial complex’s grand plan to make you paranoid. They want you to doubt every label so you’ll keep coming back. Did you know the FDA approves drug labels without testing them for legibility? And the QR codes? That’s just a tracker. They’re watching you. Always.
James Allen
December 8, 2025 AT 21:25America's pharmacies are the best in the world. You think other countries do this? Nah. We have standards. You don't need to check your label unless you're one of those people who can't follow basic instructions. If you're still worried, maybe you shouldn't be taking meds at all. Just saying.
Mary Ngo
December 9, 2025 AT 12:52The real issue here is not the label-it's the fact that your doctor’s prescription is being routed through a for-profit algorithm that prioritizes cost over safety. Generic substitutions are not neutral. They are corporate decisions disguised as clinical ones. The label is merely the symptom. The disease is profit-driven healthcare. You're being manipulated into believing the problem is your negligence. It's not. It's the system.