After surgery, pain isn’t just about the incision. Many patients struggle with cramping, bloating, and sharp abdominal spasms that feel like they’re being twisted from the inside. These aren’t normal side effects-they’re common complications caused by anesthesia, bowel manipulation, or just the body reacting to trauma. That’s where butylscopolamine comes in. It doesn’t numb pain like opioids, but it stops the muscle spasms that make pain feel unbearable. For many patients, it’s the difference between lying still and being able to breathe, sit up, or even walk a few steps without doubling over.
What Butylscopolamine Actually Does
Butylscopolamine is an antispasmodic drug. It works by blocking acetylcholine, a chemical your body uses to signal muscles to contract. In the gut, bladder, and bile ducts, this means fewer involuntary spasms. After surgery, especially abdominal or pelvic procedures, these muscles go into overdrive. The result? Severe cramping, nausea, and a feeling of pressure that mimics a bowel obstruction-even when there isn’t one.
Unlike painkillers that target nerve signals, butylscopolamine targets the root cause: muscle tension. It doesn’t make you drowsy. It doesn’t slow your breathing. It doesn’t carry the risk of addiction. That’s why it’s often given alongside opioids-not to replace them, but to make them work better.
Why It’s Used After Surgery
Surgery disrupts normal gut function. Anesthesia slows peristalsis-the wave-like motion that moves food through your intestines. When it restarts, it often does so unevenly, causing painful contractions. In gallbladder or bowel surgery, the organs are handled, stretched, or temporarily stopped. This triggers a reflexive spasm response that can last for hours or even days.
Studies from the Journal of Clinical Anesthesia show that patients given butylscopolamine after laparoscopic surgery reported 40% less abdominal discomfort within the first 24 hours compared to those who received a placebo. They also needed fewer additional doses of pain medication. That’s not just comfort-it’s faster recovery.
How It’s Given and When
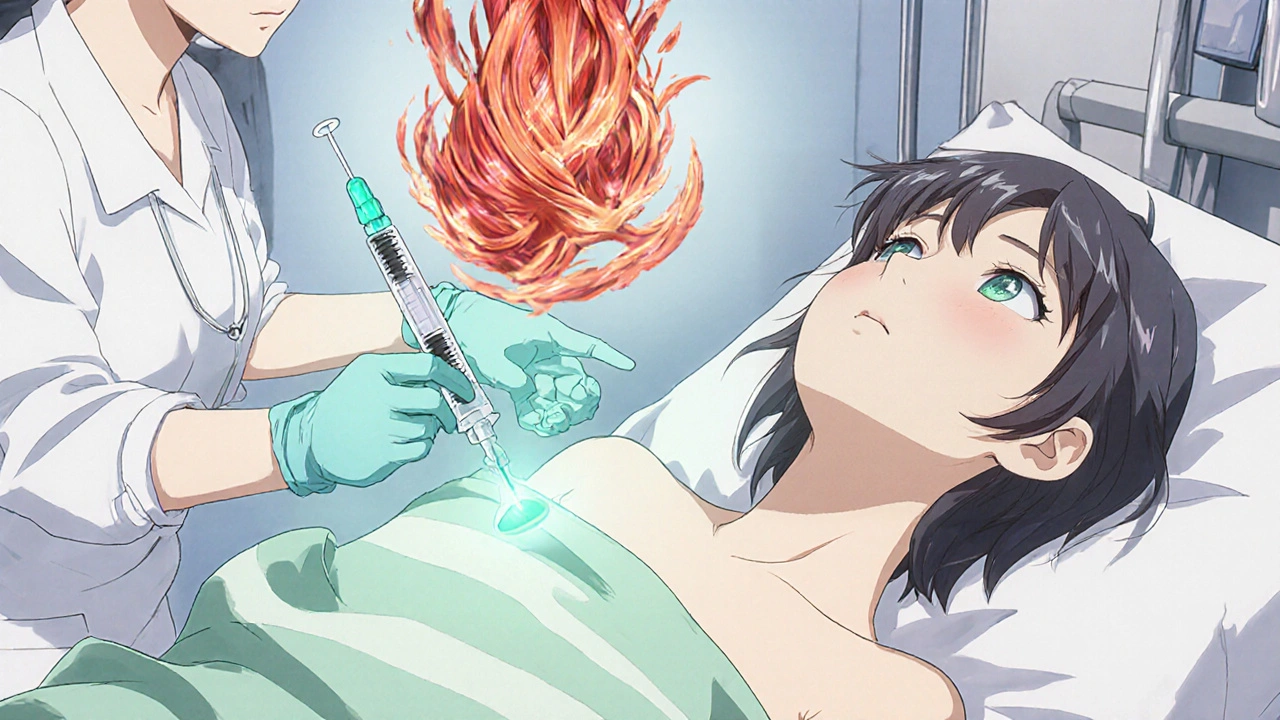
Butylscopolamine is usually administered as an injection right after surgery, either in the recovery room or during the procedure itself. Some hospitals use it as a routine part of post-op care, especially after procedures like appendectomy, hysterectomy, or bowel resection. In some cases, it’s given as a tablet or suppository if the patient is stable and able to take oral meds.
The standard dose is 20 mg intramuscularly, repeated every 6 to 8 hours if needed. It kicks in within 15 to 30 minutes and lasts about 4 to 6 hours. That timing matches up well with the peak of post-op spasms, which usually hit 1 to 3 hours after anesthesia wears off.
Who Benefits the Most
Not everyone needs it. But certain patients see dramatic results:
- Those who had abdominal or pelvic surgery
- Patients with a history of irritable bowel syndrome or chronic spasms
- People who experience severe nausea or vomiting after anesthesia
- Anyone who complains of cramping that doesn’t improve with standard painkillers
One nurse in Toronto told me about a 68-year-old woman who had a colectomy. She was on morphine but still couldn’t sit up because of cramping. After one shot of butylscopolamine, she sat up, drank water, and asked for her phone. That’s the kind of moment that changes how you think about pain management.
Side Effects and Safety
Butylscopolamine is generally safe. The most common side effects are dry mouth, blurred vision, and mild dizziness-usually temporary. It’s not recommended for people with glaucoma, urinary retention, or severe heart conditions. If you’re allergic to scopolamine or other anticholinergics, you should avoid it.
It doesn’t interact badly with most common post-op meds, including antibiotics, acetaminophen, or low-dose opioids. But it should never be mixed with other anticholinergic drugs like some antihistamines or tricyclic antidepressants without medical supervision.
How It Compares to Other Options
| Treatment | Works on | Onset | Duration | Main Side Effects |
|---|---|---|---|---|
| Butylscopolamine | Muscle spasms in gut, bladder, bile ducts | 15-30 min | 4-6 hours | Dry mouth, blurred vision |
| Hyoscine (scopolamine) | Same as butylscopolamine | 20-40 min | 6-8 hours | More drowsiness, confusion in elderly |
| NSAIDs (ibuprofen) | Inflammation, mild pain | 30-60 min | 4-6 hours | Stomach upset, bleeding risk |
| Opioids (morphine) | Nerve pain | 10-20 min | 3-5 hours | Drowsiness, constipation, addiction risk |
Butylscopolamine isn’t a painkiller. It’s a muscle relaxant for internal organs. That’s why it’s often paired with acetaminophen or low-dose opioids. Together, they cover both the nerve pain and the muscle cramping. Using just opioids leaves patients stuck with spasms that don’t respond to opioids at all.
Real-World Impact on Recovery
When spasms are controlled, patients move sooner. They breathe deeper. They eat earlier. They go home faster. One 2024 audit from a major Canadian hospital found that patients who received butylscopolamine after bowel surgery had an average hospital stay 1.2 days shorter than those who didn’t. That’s not just comfort-it’s cost savings and reduced risk of complications like pneumonia or blood clots from lying still too long.
It’s also a quiet win for mental recovery. Many patients fear the pain after surgery more than the surgery itself. When they realize they can breathe without pain, they feel more in control. That reduces anxiety, which in turn lowers cortisol levels and helps the body heal.

When It’s Not the Right Choice
Butylscopolamine won’t help with incisional pain, nerve pain from a hernia repair, or joint stiffness after hip surgery. It’s specific to smooth muscle spasms. If your pain is sharp, localized, and worsens with movement, it’s likely not spasms-it’s something else. Always tell your doctor what the pain feels like. Is it crampy? Bloating? Does it come in waves? That helps them decide if butylscopolamine is right for you.
It’s also not for long-term use. Once the gut starts moving normally again-usually within 2 to 3 days-it’s no longer needed. Overuse can lead to constipation or urinary retention, especially in older adults.
What Patients Should Ask
If you’re scheduled for surgery, ask:
- Will I be offered an antispasmodic like butylscopolamine after the procedure?
- What are the signs that I might need it?
- Can I get it as a tablet if I’m not in pain right after surgery?
- Are there any reasons I shouldn’t get it based on my medical history?
Most hospitals don’t automatically explain it. But if you ask, you’re more likely to get it. And if you’re still in pain after the first dose, speak up. Sometimes it takes two doses to fully relax the muscles.
Is butylscopolamine the same as hyoscine?
They’re very similar-both are anticholinergics that relax smooth muscles. Butylscopolamine is a synthetic version of hyoscine (scopolamine), designed to be more targeted to the gut and have fewer effects on the brain. That means less drowsiness and confusion, especially in older patients. In practice, doctors often choose butylscopolamine for post-op use because it’s safer and just as effective.
Can I take butylscopolamine at home after surgery?
It’s rarely prescribed for home use. It’s usually given in the hospital during the critical first 24-48 hours when spasms are worst. If you’re still having severe cramping at home, contact your surgeon. They may recommend other options like gentle heat, walking, or a different medication. Don’t try to get it without a prescription-it’s not available over the counter.
Does butylscopolamine help with nausea?
Not directly. But by reducing gut spasms, it can ease the feeling of nausea that comes with abdominal cramping. It’s not a substitute for anti-nausea drugs like ondansetron, but many patients report feeling less nauseous once their spasms are under control.
How long do the side effects last?
Most side effects like dry mouth or blurred vision clear up within a few hours after the last dose. They’re usually mild and don’t interfere with daily activities. If you feel confused, have trouble urinating, or your heart races, let your nurse or doctor know right away.
Is butylscopolamine used for children after surgery?
Yes, but with caution. It’s sometimes used in pediatric patients after abdominal surgery, especially for conditions like intussusception or appendectomy. Dosing is based on weight, and it’s only given under close monitoring. Pediatric use is less common than in adults, but it’s well-documented in clinical guidelines.
Final Thoughts
Post-operative pain isn’t one thing. It’s a mix of tissue injury, inflammation, and muscle spasms. Most treatments focus on just one part. Butylscopolamine fills a gap no opioid or NSAID can reach. It’s not flashy. It’s not new. But for patients stuck in cramping pain after surgery, it’s often the quiet hero that lets them finally relax-and heal.


Vishnupriya Srivastava
October 27, 2025 AT 13:29Butylscopolamine is just another anticholinergic band-aid. The real issue is how hospitals overuse drugs instead of addressing motility dysfunction with early ambulation and gut stimulation protocols. This drug masks symptoms while the root cause-post-op ileus-goes untreated. Data from 2022 shows hospitals that skipped routine antispasmodics and pushed walking within 4 hours had 30% lower readmission rates.
Kshitij Nim
October 28, 2025 AT 03:55Finally someone talks sense. I’ve seen nurses fight for this drug because patients are screaming in pain and opioids aren’t touching the cramps. It’s not magic-it’s physiology. If your gut’s spasming like a faulty engine, you don’t need more painkillers, you need to calm the damn muscle contractions. Give it to everyone after abdominal surgery. Period.
Scott Horvath
October 29, 2025 AT 07:18omg this is the real deal i had a laparoscopic cholecystectomy last year and i was basically paralyzed from cramping until they gave me this shot like 3 hours in and suddenly i could breathe again like i wasnt being stabbed from inside lmao
Armando Rodriguez
October 30, 2025 AT 11:21This is an excellent and clinically grounded overview. The distinction between nociceptive pain and visceral spasm is critically underappreciated in postoperative care. Integrating butylscopolamine into standard protocols represents a paradigm shift toward precision symptom management rather than broad-spectrum analgesia. I applaud the inclusion of comparative data and patient-centered outcomes.
jennifer sizemore
November 1, 2025 AT 07:11I’m a nurse in a trauma unit and I swear by this stuff. One time a guy came in after a bowel resection and was sobbing because he couldn’t even take a deep breath. We gave him 20mg and he just… stopped crying. Looked at me like ‘what just happened?’ That’s the moment you realize medicine isn’t always about big flashy treatments. Sometimes it’s just… letting the body relax.
matt tricarico
November 2, 2025 AT 20:31How convenient that Big Pharma pushes this as a ‘quiet hero’ when it’s just a repackaged anticholinergic with a marketing budget. You’re ignoring the fact that this drug increases delirium risk in the elderly and masks signs of anastomotic leaks. The real ‘hero’ here is clinical judgment-not another drug to throw at every post-op patient like a magic bullet.
Patrick Ezebube
November 4, 2025 AT 17:55They’re using this because it’s cheaper than real rehab. You think they care about your gut spasms? Nah. They want you out the door by day two so they can bill another patient. This drug keeps you quiet while they cut corners. And don’t get me started on how it’s linked to long-term cognitive decline in people over 60. They’re drugging you to make the system look efficient.
Kimberly Ford
November 4, 2025 AT 23:30For anyone reading this and wondering if this applies to you-yes, if you’ve ever had surgery and felt like your insides were being twisted in a washing machine, this is probably what you needed. I’ve had two surgeries and only one time they gave me this. The difference was night and day. Ask for it. Don’t wait for them to offer it. And if your pain feels crampy, not sharp-that’s the clue.
jerry woo
November 6, 2025 AT 12:47Let’s be real-this drug’s the unsung badass of post-op care. While everyone’s chasing opioids like they’re candy, this little guy silently nukes the visceral spasms that make you feel like your colon is staging a coup. No sedation. No respiratory depression. Just pure, unapologetic smooth-muscle domination. It’s the silent ninja of the ICU-quiet, efficient, and devastatingly effective. Why isn’t this on every post-op checklist? Because medicine loves complexity over simplicity. And also because no one wants to admit that sometimes, the best solution is just… stop the damn cramping.
Jillian Fisher
November 8, 2025 AT 05:23Just curious-has anyone seen data on how often this is given to patients who don’t actually have spasms? Like, is it just routine because it’s ‘safe’ or are providers actually assessing symptoms first? I’ve seen it handed out like aspirin and I wonder if we’re overusing it.