Most people hear "COPD" and think of one thing: trouble breathing. But COPD isn’t a single disease. It’s made up of two very different conditions-chronic bronchitis and emphysema-that often show up together but demand very different approaches to treatment. If you or someone you care about has been diagnosed with COPD, understanding the difference between these two isn’t just academic. It could mean the difference between fewer hospital visits, better symptom control, and a more active life.
What Exactly Is COPD?
COPD stands for Chronic Obstructive Pulmonary Disease. It’s not asthma. It’s not just "smoker’s cough." It’s a group of lung diseases that make it hard to breathe because air can’t flow in and out of the lungs properly. Around 380 million people worldwide have it, and it’s the fourth leading cause of death globally. In the U.S. alone, about 16 million people are diagnosed, and many more likely have it but haven’t been tested.
The two main components are chronic bronchitis and emphysema. You can have one, the other, or both. And while they both cause shortness of breath, the way they damage your lungs-and how you treat them-is completely different.
Chronic Bronchitis: The Mucus Problem
Chronic bronchitis is defined by one simple, persistent symptom: a productive cough that lasts at least three months a year for two years in a row. That means you’re coughing up mucus-often a lot of it. Daily. For years.
Inside your airways, the lining becomes inflamed. The mucus-producing cells (goblet cells) multiply by 300 to 500%, and the glands beneath them swell up. Instead of producing 10 to 100 milliliters of mucus a day like a healthy lung, a chronic bronchitis lung can make 100 to 200 mL. That’s a quarter of a cup of thick, sticky mucus every day.
That mucus doesn’t just sit there. It clogs the small airways. You feel it when you try to take a deep breath. You hear it when you clear your throat in the morning. Some patients report spending 20 to 30 minutes every day doing chest physiotherapy just to clear it out. One Reddit user measured his morning mucus output with a measuring cup-100 mL, every day, for eight years.
People with chronic bronchitis are often called "blue bloaters." That’s because their blood oxygen levels drop (85-89%), leading to a bluish tint around the lips or fingernails (cyanosis). Their bodies are working overtime to get oxygen, which strains the heart. Many develop cor pulmonale-a form of heart failure caused by lung disease-which leads to swollen ankles and legs.
Emphysema: The Air Sac Collapse
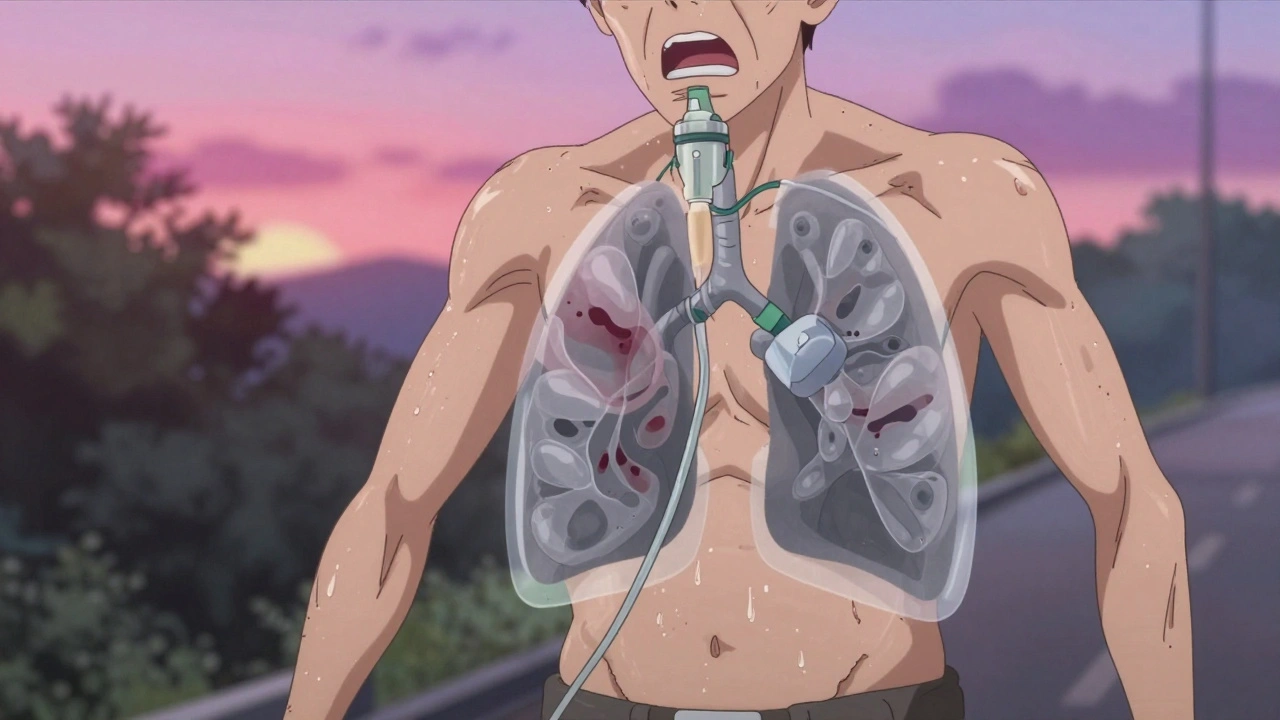
Emphysema is the silent destroyer. There’s no constant cough. No thick mucus. Instead, the tiny air sacs in your lungs-the alveoli-start to break down. These sacs are what let oxygen into your blood and remove carbon dioxide. When they’re destroyed, they don’t regenerate. You lose 30 to 50% of your lung’s natural elasticity.
Imagine a balloon that’s been stretched too many times. It loses its shape. That’s your lung. The walls between air sacs collapse, forming large, inefficient air spaces. Your lungs can’t push air out properly. You’re left feeling like you’re constantly gasping for air-even when you’re sitting still.
This is the "pink puffer" phenotype. These patients are often thin, breathe fast (25-30 breaths per minute), and have a barrel-shaped chest because their lungs are overinflated. Their skin stays pink because they’re hyperventilating to compensate. Their oxygen levels might even stay normal (92-95%)-but only because they’re working so hard.
Emphysema doesn’t make you cough up mucus. It makes you run out of breath. Fast. You can’t talk in full sentences. You stop after five or six words. Walking up a hill becomes impossible. Eventually, even walking across the room feels like climbing a mountain.
How Doctors Tell Them Apart
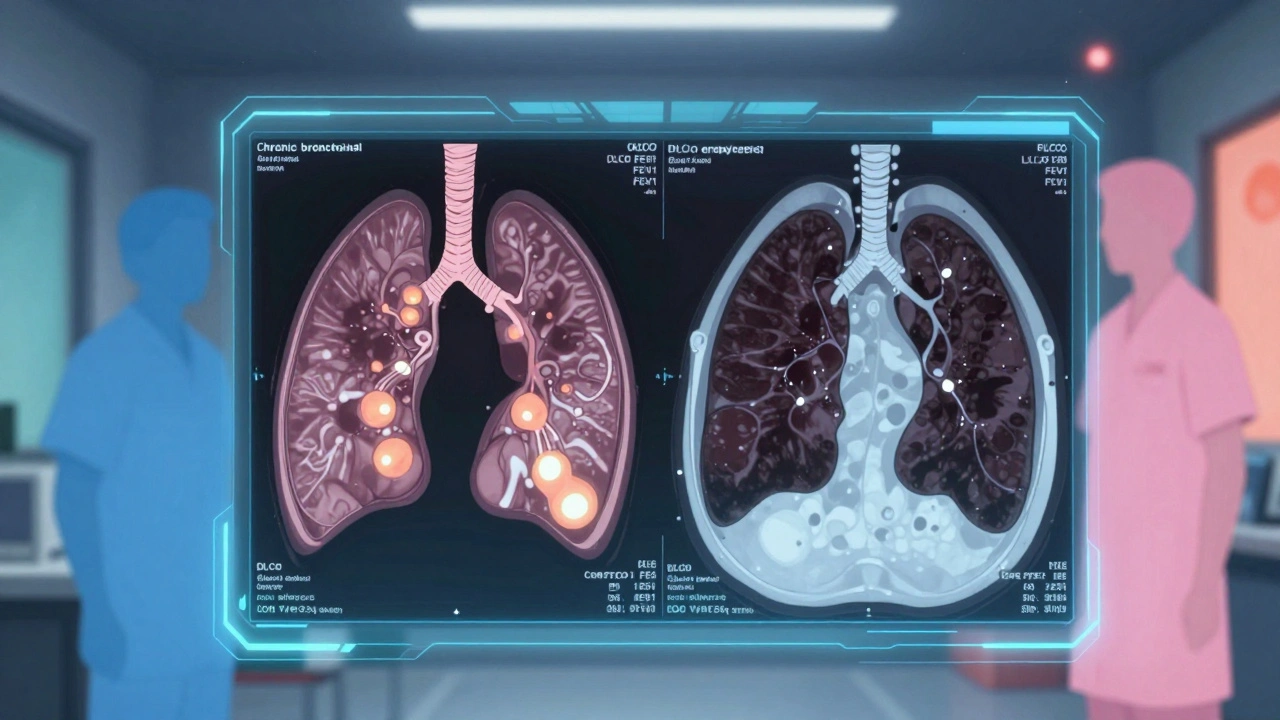
There’s no single test that gives you a label. But pulmonologists use a combination of tools to figure out which component dominates.
- Pulmonary Function Tests (PFTs): Both show low FEV1/FVC ratio (below 70%), meaning airflow is blocked. But emphysema shows a low DLCO-diffusing capacity for carbon monoxide. If it’s under 60% of predicted, emphysema is likely the main issue.
- CT Scans: High-resolution scans show emphysema as dark, low-density areas covering more than 15% of the lung. Chronic bronchitis shows thickened airway walls-over 60% wall area on expiratory scans.
- 6-Minute Walk Test: Emphysema patients drop their oxygen saturation below 88% within two minutes. Chronic bronchitis patients stay oxygenated but stop because they’re out of breath.
And here’s the catch: 85% of people with severe COPD have features of both. Only 15% have pure chronic bronchitis or pure emphysema. But even in mixed cases, one side usually dominates-and that’s what guides treatment.
Treatment: One Size Does NOT Fit All
This is where most patients get lost. If your doctor just says "take your inhalers," they’re not treating the disease-they’re treating the label. The right treatment depends on which part of COPD you have.
For chronic bronchitis:
- Mucolytics like carbocisteine reduce mucus thickness and cut exacerbations by 22%.
- Hypertonic saline nebulizers (saltwater mist) help loosen mucus-73% of users report better clearance.
- If you have more than two flare-ups a year, roflumilast (a pill) can reduce them by 17.3%.
- Avoid inhaled steroids. They increase pneumonia risk by 40% in chronic bronchitis patients.
- First-line treatment: LAMA/LABA combo inhalers (like Anoro or Stiolto).
For emphysema:
- Lung volume reduction surgery or endobronchial valves can improve breathing by 35% in those with upper-lobe disease and FEV1 under 35%.
- If you have alpha-1 antitrypsin deficiency (1-2% of emphysema cases), weekly infusions of the missing protein can slow lung damage.
- Inhaled alpha-1 antitrypsin, approved by the FDA in 2023, showed a 20% improvement in FEV1 after 12 months.
- Portable oxygen helps, but it’s heavy. Many patients say it limits their mobility-even with modern concentrators delivering 2-4 liters per minute.
A 2022 study in the New England Journal of Medicine found that patients who got treatment matched to their COPD component had 27% fewer hospital stays than those who didn’t. That’s not a small difference. That’s life-changing.
What Happens If You Don’t Know the Difference?
Too many patients get antibiotics every time they feel worse-even if their cough isn’t caused by infection. That’s common in chronic bronchitis, but unnecessary. Antibiotics don’t reduce mucus. They just add side effects.
Or worse-emphysema patients get stuck on steroid inhalers, which do nothing for their air sac damage and raise their risk of pneumonia and bone loss.
Dr. Fernando Martinez, editor of the American Journal of Respiratory and Critical Care Medicine, put it bluntly: "Failing to differentiate between these phenotypes results in suboptimal therapy."
Primary care doctors miss the distinction more often than pulmonologists. A 2023 survey found only 42% of family doctors regularly differentiate between chronic bronchitis and emphysema, compared to 78% of lung specialists.
What’s New in 2025?
The field is moving fast. In 2024, a new acoustic device launched in Europe that uses sound waves to shake loose mucus in chronic bronchitis patients-cutting flare-ups by 32%.
For emphysema, bronchoscopic thermal vapor ablation is showing 78% success in improving lung function at two years. It’s less invasive than surgery and works by shrinking damaged areas of the lung.
Researchers are now testing blood biomarkers-like eosinophil counts above 300 cells/μL-to predict who will respond to new biologic drugs for chronic bronchitis. The NIH’s SPIROMICS-2 study is tracking 10,000 patients through 2026 to find these patterns.
And the market is responding. Drugs like ensifentrine, designed specifically for chronic bronchitis, brought in $142 million in sales in 2023. Endobronchial valve procedures jumped 22% in the U.S. last year.
Living With It
Both conditions are progressive. But they don’t have to control your life.
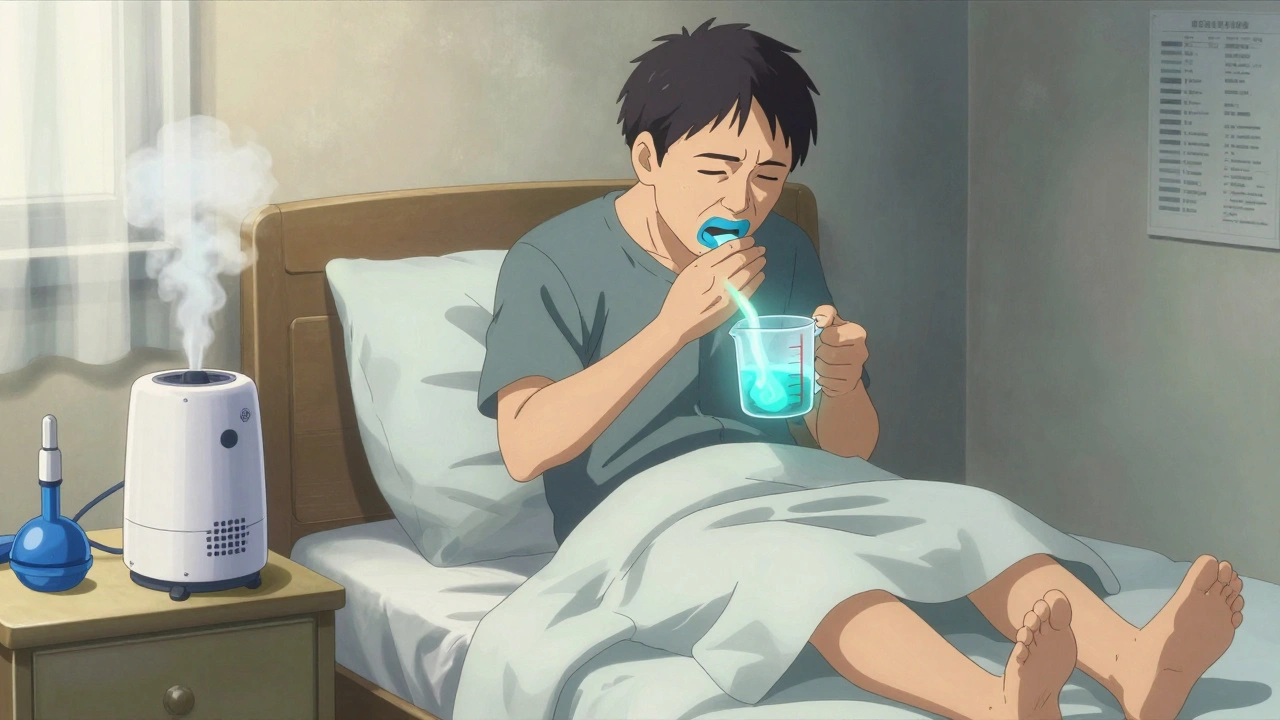
Chronic bronchitis patients benefit from daily hydration, humidifiers, and pulmonary rehab that teaches breathing techniques and mucus clearance. Many find relief with airway clearance devices like the Flutter or Acapella.
Emphysema patients need to protect their lungs from cold air and pollution. Oxygen therapy helps, but mobility matters. Lightweight, portable concentrators now weigh under 5 pounds. Some patients use them on walks, even in Toronto winters.
Both groups benefit from pulmonary rehabilitation-structured exercise, education, and support. A 2022 study showed 6-minute walk distance improved by 35% after 12 weeks of rehab.
And don’t underestimate community. The COPD Foundation’s online forums and local chapters help 15,000+ patients. Eighty-seven percent say they feel more in control after six months of support.
What Should You Do Next?
If you’ve been diagnosed with COPD and no one has talked to you about whether you have more bronchitis or more emphysema, ask. Request your PFT results. Ask about your DLCO. Ask if you’ve had a CT scan. Ask if your treatment matches your phenotype.
Don’t settle for "COPD inhalers." Demand precision. Because your lungs are unique. Your treatment should be too.

John Filby
December 4, 2025 AT 17:11Man, I never realized how different these two are until I read this. My dad’s got the "pink puffer" thing-thin as a rail, always breathing hard, but never coughing up stuff. We just thought he was out of shape. Turns out he’s been mismanaged for years.
Ollie Newland
December 6, 2025 AT 09:24DLCO under 60% is the smoking gun for emphysema. If your pulmonologist isn’t checking it, find a new one. Same with high-res CT-PFTs alone are useless for phenotyping. This post nails it. I’ve seen too many patients get steroid inhalers when they need bronchodilators or even valves. It’s criminal.
Heidi Thomas
December 7, 2025 AT 21:57Antibiotics for mucus? Are you kidding me? This is why people think COPD is just "a bad cold that won’t go away." It’s not infection, it’s inflammation. Stop treating symptoms like they’re bugs.
zac grant
December 7, 2025 AT 23:25Just got my DLCO results back-48%. I thought I was just getting older. Turns out I’ve got severe emphysema. I’m gonna ask for the endobronchial valve eval next visit. Thanks for the clarity. This is the first time anyone’s explained it like this.
Gillian Watson
December 9, 2025 AT 11:26My mum’s been on carbocisteine for 3 years now. She says it’s the only thing that lets her sleep without coughing. And the hypertonic saline nebulizer? Game changer. We got one on Amazon for $80. No prescription needed. She uses it every morning before breakfast.
George Graham
December 10, 2025 AT 10:25My brother was told he had "COPD" and given a steroid inhaler. He got pneumonia three times in a year. We switched to a LAMA/LABA combo after reading this. He hasn’t been hospitalized since. This isn’t just info-it’s life-saving.
Jordan Wall
December 11, 2025 AT 08:57Ugh, yet another post pretending to be "medical wisdom" but really just regurgitating 2023 guidelines. Did you even read the GOLD 2024 update? They now classify COPD by exacerbation frequency, not phenotype. Also, bronchoscopic ablation? That’s still Phase 3. Stop overselling. 🤦♂️
Dematteo Lasonya
December 12, 2025 AT 01:05I’m a nurse in a pulmonary clinic and I see this every day. Patients get labeled COPD and handed a blue inhaler like it’s a magic pill. No one asks if they’re coughing up soup or gasping at the mailbox. This breakdown is exactly what we need more of.
Alex Piddington
December 12, 2025 AT 21:14Thank you for this comprehensive and compassionate overview. The emphasis on phenotyping over labeling is critical. I’ve shared this with my entire care team. We’re now incorporating DLCO and CT review into our COPD intake protocol. Small changes, big impact.
Scott van Haastrecht
December 14, 2025 AT 19:11Everyone’s acting like this is some groundbreaking revelation. Newsflash: we’ve known this since the 80s. The real problem? Doctors are lazy. They don’t want to do the work. They don’t want to read PFTs or order CTs. So they just hand out inhalers and call it a day. This post doesn’t fix the system. It just points out the obvious. And you’re all patting yourselves on the back like you just solved cancer.
Rudy Van den Boogaert
December 15, 2025 AT 14:44I’ve got both, but bronchitis dominates. I use the Flutter device every morning. Takes 10 minutes. Feels like I’m breathing again. Also, the new ensifentrine? My pulmonologist put me on it last month. My FEV1 jumped 12%. I’m not gonna lie-I cried. After 12 years of feeling like I was drowning, I finally feel like I’m not fighting just to get air.
Libby Rees
December 16, 2025 AT 18:32Ask for your DLCO. Ask for your CT. Ask if your treatment matches your phenotype. That’s it. That’s the whole post. Short. Clear. Necessary. Thank you.