Imagine being told you have lupus, then months later, your fingers start tightening like rubber bands. Then your muscles ache so badly you can’t lift a coffee cup. Your doctor checks your blood again-now there’s a new antibody. You’re not getting worse. You’re getting overlap. This isn’t rare. It’s not a mistake. It’s autoimmune overlap syndrome.
More than 1 in 4 people with a known autoimmune disease like lupus, scleroderma, or rheumatoid arthritis will eventually develop signs of another. These aren’t random coincidences. They’re real, measurable conditions where the immune system attacks multiple tissues at once. And they’re harder to diagnose, treat, and manage than any single disease.
What Exactly Is an Autoimmune Overlap Syndrome?
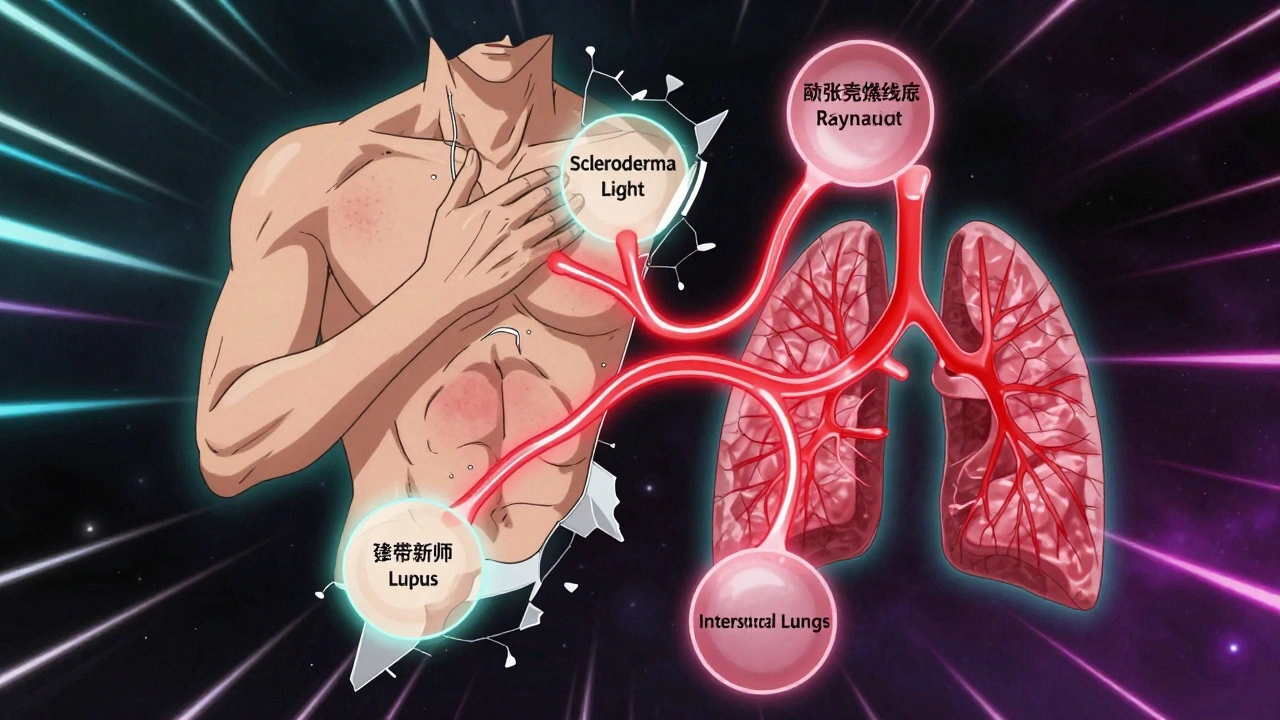
An autoimmune overlap syndrome happens when someone meets the official diagnostic criteria for two or more distinct autoimmune connective tissue diseases. The big five are: systemic lupus erythematosus (SLE), scleroderma, polymyositis, rheumatoid arthritis, and Sjögren’s syndrome. When symptoms from two or more show up together, it’s not just "a bit of everything." It’s a specific pattern with its own rules.
One of the most studied is mixed connective tissue disease (MCTD). People with MCTD have high levels of anti-U1-RNP antibodies-often over 1:10,000. They usually get puffy hands, Raynaud’s (fingers turning white in the cold), swollen joints, and muscle weakness. But they don’t always get the kidney damage or severe rashes typical of lupus. That’s the key: MCTD isn’t lupus plus scleroderma. It’s its own thing, with its own antibody signature.
Then there’s antisynthetase syndrome. This one is tied to antibodies like anti-Jo-1. People here often get inflamed muscles (myositis), scarring in the lungs (interstitial lung disease), and rough, cracked skin on their fingers-called mechanic’s hands. About 70% of these patients have lung involvement, which can be life-threatening if missed.
Polymyositis/scleroderma (PM/Scl) overlap shows up in people with muscle weakness and skin thickening-but not the classic digital ulcers or pulmonary hypertension of pure scleroderma. And then there’s Multiple Autoimmune Syndrome (MAS), where three or more autoimmune diseases cluster together. Type 2 MAS might include Sjögren’s, rheumatoid arthritis, and thyroid disease. Type 3 can involve diabetes, vitiligo, and lupus all at once.
Why Diagnosis Takes So Long
Doctors aren’t slow on purpose. The problem is that the rules for diagnosing each disease were made for single conditions. When symptoms bleed together, those rules break down.
For example, if you have joint pain and fatigue, you might be labeled with lupus. But if your skin starts tightening and your lungs show early scarring, that’s not classic lupus. It’s PM/Scl overlap. Yet many rheumatologists wait until all criteria are met-sometimes for years-before changing the diagnosis.
A 2022 study found that 45% of patients with overlap syndromes waited over 18 months for a correct diagnosis. Compare that to 12 months for someone with just lupus. Why? Because symptoms are messy. One specialist sees the skin and thinks scleroderma. Another sees the muscle weakness and thinks myositis. No one connects the dots.
And here’s the kicker: up to 40% of people initially diagnosed with "undifferentiated connective tissue disease" (UCTD) eventually develop a clear overlap pattern within five years. So if you’ve been told you have "something unclear," don’t assume it’s nothing. It might be evolving.
What Doctors Look For: Antibodies and Imaging
Diagnosis isn’t just about symptoms. It’s about blood tests and scans.
Anti-U1-RNP is the fingerprint of MCTD. It’s present in 83% of cases and is 95% specific-meaning if it’s high, you likely have MCTD, not something else.
Anti-PM/Scl antibodies show up in 2-5% of scleroderma patients and 8-10% of polymyositis cases. They’re rare, but when found, they’re almost always linked to overlap.
Anti-Jo-1 is the hallmark of antisynthetase syndrome. It’s found in 75-80% of cases. Other synthetase antibodies like anti-PL-7 and anti-PL-12 are less common but just as important.
But antibodies alone aren’t enough. Lung scans are critical. Up to 70% of antisynthetase patients and 50% of PM/Scl patients develop interstitial lung disease (ILD). That’s why EULAR guidelines now say: if you suspect any overlap, get a high-resolution CT scan of the lungs and pulmonary function tests. Missing ILD can be deadly.
How Treatment Is Different
Treating one autoimmune disease is hard. Treating two or more at once? It’s like balancing five balls in the air while riding a bike.
The first line is usually low-dose steroids (like prednisone) plus one immunosuppressant-methotrexate or mycophenolate. But here’s where it gets tricky: what if your lungs are failing but your joints are fine? You can’t treat the joints the same way you treat the lungs.
For ILD, rituximab has become a game-changer. Given as two IV infusions every six months, it stabilizes or improves lung function in 60-70% of patients with antisynthetase syndrome. In March 2023, the FDA even approved tocilizumab specifically for this type of lung scarring.
But here’s the danger: doctors sometimes pile on drugs. One for the skin, one for the joints, one for the lungs. A 2019 study found that 35% of overlap patients end up on three or more immunosuppressants. That’s a recipe for infections. People on triple therapy have nearly double the risk of serious infections compared to those on one or two drugs.
The goal isn’t to hit every symptom with a hammer. It’s to identify the most dangerous or disabling feature-and treat that first.
The Real Problem: Care That Doesn’t Talk to Itself
The biggest barrier isn’t medicine. It’s the system.
Patients often see a rheumatologist for lupus, a pulmonologist for lung issues, a dermatologist for skin changes, and a neurologist if they have nerve problems. No one talks to each other. Appointments are scattered. Medications aren’t reviewed together. Side effects pile up.
One patient on Reddit wrote: "I see seven specialists. None of them know what the others are prescribing. I’m taking 11 pills a day and still feel awful."
At the Cleveland Clinic’s Overlap Syndrome Program, they fixed this with one role: a care coordinator. This person schedules all appointments, tracks medications, reviews labs, and acts as the patient’s single point of contact. The result? Hospitalizations dropped by 35%. Medication adherence jumped 42%.
Specialized centers like Johns Hopkins, Mayo Clinic, and Hospital for Special Surgery are leading the way. But most community hospitals still treat overlap syndromes as a collection of separate diseases.
What’s Changing Now
There’s real progress. In 2023, the NIH launched a $15 million project to find biomarkers that predict which patients will develop overlap syndromes-and how fast. That could mean earlier intervention.
AI is also stepping in. A 2022 study used machine learning to analyze electronic health records and predicted overlap syndromes 12 months before doctors noticed symptoms. Accuracy? 82%.
The American College of Rheumatology updated its guidelines in June 2023 to include "treat-to-target" goals: keep lung function above 80% predicted, keep skin thickening below a certain score, and aim for minimal disease activity in joints. These aren’t vague ideas. They’re measurable targets.
And the market is responding. Drug development for overlap syndromes is growing at 7.2% per year. Anifrolumab, a drug approved for lupus, is now in phase 2 trials for MCTD. That’s the first time a drug is being tested specifically for an overlap condition.
What Patients Should Do
If you have an autoimmune disease and new symptoms show up-especially lung problems, muscle weakness, or skin changes that don’t fit your original diagnosis-ask: "Could this be an overlap?"
Request testing for specific antibodies: anti-U1-RNP, anti-Jo-1, anti-PM/Scl. Ask for a high-resolution CT scan of your lungs. Don’t wait for symptoms to get worse.
Ask your doctor if you can be referred to a center with a dedicated overlap syndrome program. If your care feels fragmented, ask for a care coordinator. You have the right to ask for one.
Keep a symptom journal. Note when your fingers turn white, when your muscles feel weak, when your breathing changes. Bring it to every appointment. You’re the expert on your body.
And remember: you’re not imagining things. You’re not "just having bad luck." You have a real, complex condition that’s only now starting to get the attention it deserves.
Can you have autoimmune overlap syndromes without a positive antibody test?
Yes, but it’s rare. Most overlap syndromes are defined by specific autoantibodies. However, some patients show clear clinical features-like muscle weakness plus skin tightening-but test negative for known antibodies. These cases are often called "seronegative overlap." They’re harder to classify, but still treated based on symptoms and organ involvement. Ongoing research is looking for new antibodies in these patients.
Is overlap syndrome hereditary?
Autoimmune diseases in general run in families, but overlap syndromes themselves aren’t directly inherited. If you have a close relative with lupus or scleroderma, your risk of developing *any* autoimmune disease is higher. But whether it turns into one disease or an overlap depends on a mix of genes, environment, and immune triggers-not a single inherited gene.
Can stress trigger an autoimmune overlap?
Stress doesn’t cause autoimmune diseases, but it can push them into action. Many patients report a major life stressor-like surgery, infection, or emotional trauma-preceding the start of new symptoms. Stress hormones can activate immune cells in ways that make existing autoimmunity worse or spread to new tissues. Managing stress isn’t a cure, but it’s part of keeping the immune system from going into overdrive.
Are biologics safe for overlap syndromes?
Biologics like rituximab and tocilizumab are increasingly used and often effective, especially for lung involvement. But they’re not risk-free. Because overlap syndromes involve multiple systems, a drug that helps one part might worsen another. For example, a biologic that works well for joint inflammation might not help-and could even trigger-lung scarring in some cases. Treatment must be carefully tailored and monitored.
How do I know if I need a specialist instead of a general rheumatologist?
If you’ve been diagnosed with two or more autoimmune conditions, or if your symptoms don’t fit neatly into one category, you likely need a specialist in connective tissue diseases. Look for a rheumatologist who works at a major academic medical center or has a focus on overlap syndromes. Ask if they’ve treated more than 10 patients with MCTD, antisynthetase syndrome, or PM/Scl overlap. Experience matters.


Webster Bull
December 13, 2025 AT 15:39Overlap syndromes are real. Stop acting like it's just 'bad luck.' Your body's not broken-it's just fighting on too many fronts.
kevin moranga
December 15, 2025 AT 06:31I’ve been living with MCTD for 8 years now. At first, I thought the joint pain was just lupus flaring. Then came the Raynaud’s, then the muscle weakness so bad I couldn’t open jars. My doctor kept saying ‘it’s just lupus getting worse.’ It wasn’t. It was my immune system throwing a full-blown party and inviting every autoimmune disorder it knew. The anti-U1-RNP test was the key-I’d had it done once years ago and it was negative. They redid it after I begged. Boom. 1:15,000. That’s when everything changed. Now I’m on rituximab and my lungs are stable. I still get tired, still have days where my hands feel like they’re wrapped in plastic, but I’m alive. And I’m not alone. There are thousands of us out here, just trying to get someone to listen. Don’t wait for the perfect test. If your symptoms don’t fit the box, ask if the box is the problem.
Donna Hammond
December 15, 2025 AT 14:06As someone who works in rheumatology, I see this every day. The biggest tragedy isn’t the disease-it’s the delay. Patients get passed from specialist to specialist like a hot potato. One sees skin, one sees lungs, one sees joints. Nobody sees the whole picture. We need more care coordinators. We need systems that treat the patient, not the label. I’ve had patients come in with 12 medications, no one knowing why they’re on them. It’s not just ineffective-it’s dangerous. The fact that AI can predict overlap 12 months before diagnosis should be a wake-up call. We’re not falling behind because we’re dumb-we’re falling behind because our systems are broken.
Bruno Janssen
December 16, 2025 AT 01:02I used to think I was strong. Now I know I’m just stubborn. I’ve been on prednisone for 4 years. My bones are crumbling. My stomach’s in ruins. I cry in the shower because I can’t lift my kid. And no one gets it. Not even my family. They say ‘at least you’re not dead.’ Yeah. Thanks.
Scott Butler
December 16, 2025 AT 18:06This is why America’s healthcare is a mess. You let people get diagnosed with five diseases at once because no one wants to take responsibility. In my country, they’d have just one doctor who knew what to do. Here? You need a PhD just to get your meds sorted.
Emma Sbarge
December 18, 2025 AT 10:20My sister had this. She was misdiagnosed for 22 months. They thought it was fibromyalgia. Then she got pneumonia and nearly died because no one checked her lungs. When they finally did the CT scan, the scarring was already advanced. She’s on oxygen now. Don’t wait. Get the scan. Ask for the antibody test. Your life depends on it.
Richard Ayres
December 18, 2025 AT 13:14The idea that autoimmune diseases can overlap in such specific, measurable patterns challenges the traditional model of disease classification. Rather than viewing them as isolated entities, we might need to reframe them as manifestations of a broader immune dysregulation spectrum. This could fundamentally alter how we approach diagnosis, treatment, and even research funding. The emergence of treat-to-target protocols and biomarker-driven prediction models suggests we are on the cusp of a paradigm shift in rheumatology-one that prioritizes systemic understanding over siloed symptom management.
Harriet Wollaston
December 20, 2025 AT 05:15I’m from a small town in Ohio. We don’t have a rheumatology center nearby. I had to drive 3 hours every month just to see someone who knew what I was talking about. My local doctor kept saying, ‘You’re just stressed.’ I cried in the parking lot before every appointment. Then I found a Reddit group. Someone there told me to ask for anti-Jo-1. I did. It was positive. That one test changed everything. You’re not crazy. You’re not exaggerating. You’re just fighting a system that wasn’t built for people like you.
Lauren Scrima
December 20, 2025 AT 10:13So let me get this straight… you’re telling me that instead of one disease, I have THREE? And the only reason I didn’t get diagnosed sooner is because doctors don’t like messy cases? Wow. Just… wow. I’m glad my insurance doesn’t cover sarcasm.
sharon soila
December 21, 2025 AT 10:34Every person deserves to be seen. Every symptom matters. Your body is not broken-it is speaking. And if no one is listening, you must keep speaking louder. You are not alone. You are not too much. You are not a burden. You are a warrior. And warriors don’t wait for permission to fight. Get the scan. Ask for the test. Find your team. Your life is worth every step.
Hamza Laassili
December 22, 2025 AT 21:47Y’all are overcomplicating this. Just get the antibody test. If it’s positive, you got overlap. If it’s not, you still got something. Stop waiting for someone to give you a label. You know your body better than any doctor who only sees you for 12 minutes. Go get the CT. Go ask for rituximab. Don’t wait. Your lungs don’t care about your insurance.