Ascites Management: What Works, What to Avoid, and How to Stay Safe
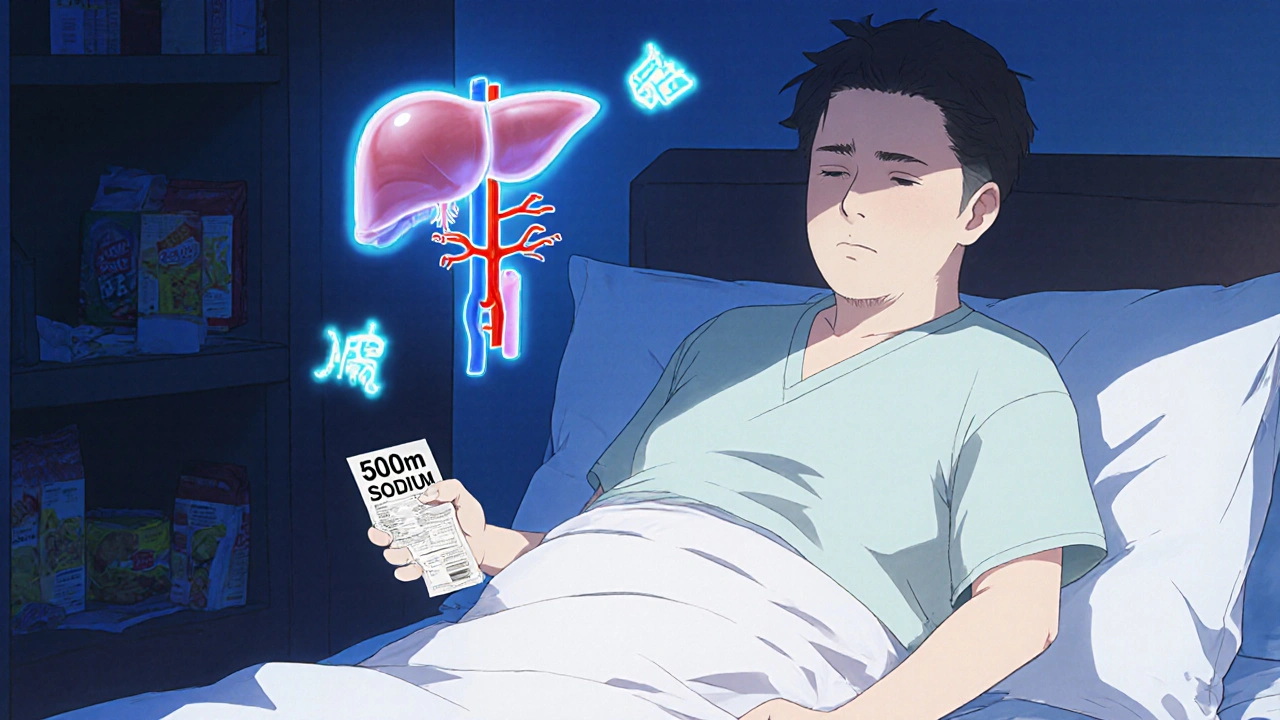
When fluid builds up in the belly—called ascites, an abnormal collection of fluid in the abdominal cavity, often linked to liver disease—it’s not just uncomfortable. It can mean your liver isn’t working right, your kidneys are under stress, or your body’s fluid balance is broken. Ascites doesn’t show up out of nowhere. It’s usually a sign of something deeper, like liver cirrhosis, scarring of the liver that impairs function and increases pressure in the portal vein, or sometimes heart or kidney problems. Treating the swelling without fixing the cause is like mopping the floor while the sink keeps overflowing.
Effective ascites management starts with three pillars: cutting back on salt, using the right diuretics, and knowing when to drain the fluid. Most people with ascites need to stay under 2,000 mg of sodium a day—not because it’s trendy, but because too much salt makes your body hold onto water like a sponge. Diuretics like spironolactone and furosemide are the go-to, but they’re not one-size-fits-all. Taking them wrong can zap your potassium, mess with your kidneys, or make you dizzy and fall. And while draining fluid with a needle—called paracentesis, a procedure to remove excess fluid from the abdomen using a thin needle—gives quick relief, it’s not a cure. Repeated paracentesis without addressing the root issue can lead to infection, low blood pressure, or even kidney failure.
People with ascites often get caught in a cycle: fluid builds up, they feel bloated, they eat less, they lose muscle, and their body gets weaker. That’s why nutrition and movement matter as much as pills. Protein intake helps keep fluid from leaking out of blood vessels. Light walking improves circulation and reduces swelling. And skipping alcohol? Non-negotiable. If you’re on multiple meds for other conditions—like high blood pressure or diabetes—watch for interactions. Some drugs make ascites worse, especially NSAIDs like ibuprofen. Your pharmacist can help you sort that out.
What you won’t find in most guides: how to tell if your ascites is getting dangerous. Sudden weight gain over a few days, sharp belly pain, fever, or confusion could mean spontaneous bacterial peritonitis—an infection inside the fluid. It’s rare but deadly if missed. Blood tests and fluid analysis are the only way to confirm it. That’s why regular check-ins with your doctor aren’t optional. They’re lifesaving.
Below, you’ll find real-world advice from people who’ve walked this path. Some posts break down which diuretics work best when cirrhosis is involved. Others show how to track fluid at home without a scale. One even explains why some patients get better with just salt control and no pills at all. These aren’t theory pieces. They’re practical, tested, and focused on what actually changes outcomes—not just symptoms.