When your eye doctor says they need to take images of your retina, it’s not just a quick snapshot. It’s a deep dive into the health of the back of your eye - and the difference between catching a problem early or missing it entirely. Three tools dominate this space today: OCT, fundus photography, and fluorescein angiography. Each shows something different. Together, they paint a full picture of what’s happening inside your eye.
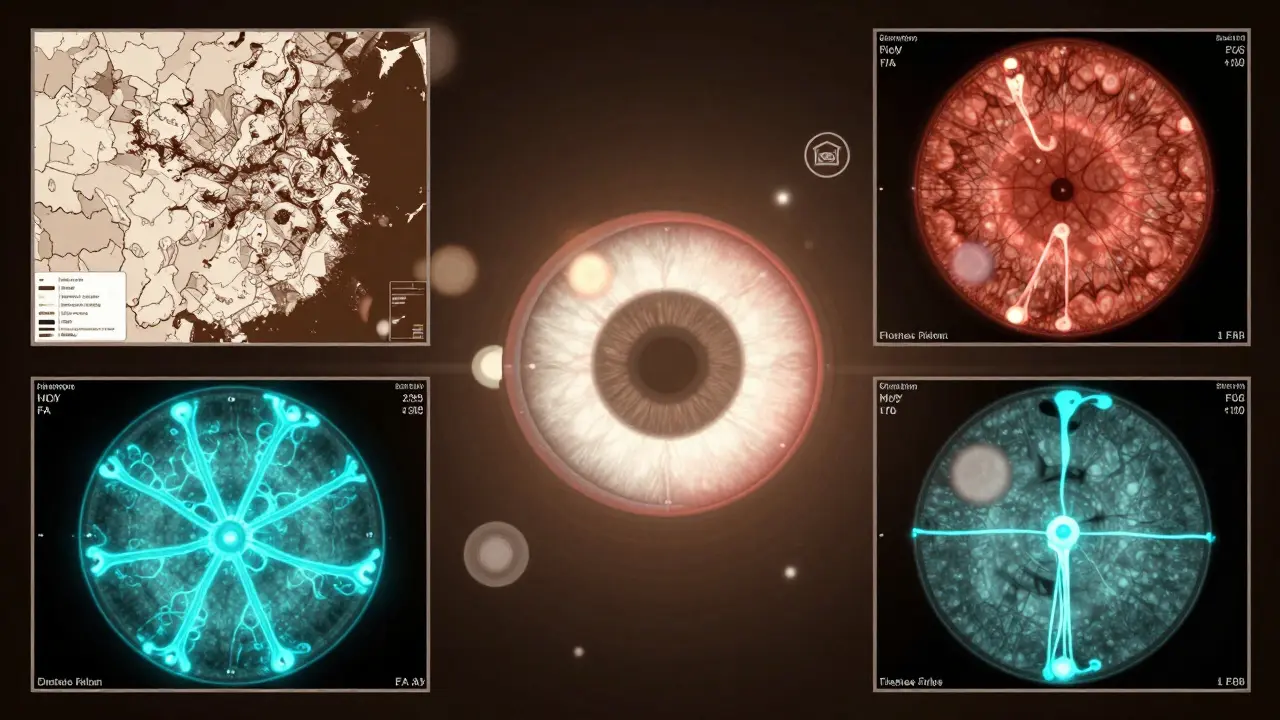
What OCT Really Shows
Optical Coherence Tomography, or OCT, doesn’t take a picture like a camera. It uses light waves to build a 3D cross-section of your retina - layer by layer. Think of it like slicing open an onion to see each layer without touching it. This is how doctors spot swelling in the macula, tiny holes, or fluid leaks long before you notice vision changes. Spectral-domain OCT (SD-OCT) has been the standard since the late 2000s. It captures images with a resolution of 5 to 7 micrometers - fine enough to see individual retinal layers. Newer swept-source OCT (SS-OCT) goes even deeper, scanning up to 400,000 times per second. That means it can see past the retina into the choroid, the layer underneath that feeds blood to the retina. This matters because conditions like choroidal neovascularization or thickened choroid layers often hide there. In diabetic retinopathy, OCT catches fluid buildup in the macula before it causes blurry vision. In age-related macular degeneration, it shows drusen deposits and thinning of the retinal pigment epithelium. For macular holes, it reveals the exact size and depth. And in Coats disease, OCT finds tiny pockets of fluid and cholesterol crystals under the retina that regular photos miss - 82% of cases showed these features only on OCT.Fundus Photography: The Big Picture
Fundus photography is what most people picture when they think of an eye exam. A flash, a bright light, and a detailed color image of your retina, optic nerve, and blood vessels. Cameras like the Zeiss FF 450+ are common in clinics. These images are used to track changes over time - a new blood vessel here, a bleed there. It’s the go-to for diabetic retinopathy screening. You can see microaneurysms, hemorrhages, and cotton wool spots clearly. But it has limits. If your pupil is small or your lens is cloudy from cataracts, the image gets blurry. It also can’t show depth. A swollen area might look like a dark spot, but you won’t know if it’s fluid, blood, or scar tissue. That’s why fundus photos are rarely used alone. They’re the map. OCT and angiography are the GPS.Fluorescein Angiography: Seeing Blood Flow
Fluorescein angiography (FA) is the only test that shows how blood moves through your retina. A yellow dye is injected into your arm, and a special camera takes rapid photos as the dye flows through your eye’s vessels. It’s like watching water move through a garden hose - you see where it leaks, where it’s blocked, or where new, abnormal vessels are growing. It’s still the gold standard for detecting leaking blood vessels in diabetic macular edema. One study found FA was 100% sensitive in spotting leakage, while OCT only caught 79%. That 21% gap? That’s where patients could be under-treated if only OCT was used. But FA has downsides. It’s invasive. You might feel nauseous. Some people get hives. Rarely, there’s a serious allergic reaction. It takes 10 to 30 minutes. And it can’t show the fine capillary networks - just the bigger vessels.
OCT Angiography: The Game Changer
OCT angiography (OCTA) is the newest player. It does what FA does - shows blood flow - but without the dye. It uses motion detection to map tiny capillaries. In seconds, you get a 3D map of the superficial, middle, and deep layers of your retina’s blood supply. For diabetic retinopathy, OCTA detects early signs of non-perfusion - areas where capillaries have shut down - before they show up on FA. In Coats disease, it finds abnormal vessels hidden under thick exudates. In punctate inner choroidopathy (PIC), OCTA spotted choriocapillaris blockages that traditional imaging completely missed. It’s faster, safer, and gives more detail than FA. But it’s not perfect. Motion artifacts from blinking or eye movement can ruin the image. It can’t detect leakage - only flow. So if a vessel is leaking fluid but still flowing, OCTA might miss it. That’s why many clinics still use FA alongside OCTA.How They Work Together
No single test tells the whole story. Here’s how they fit together:- Fundus photo gives you the overall layout: where the optic nerve is, where the macula is, if there’s a big bleed.
- OCT tells you the structure: Is the retina swollen? Are layers thinning? Is there fluid under the retina?
- Fluorescein angiography shows you the leaks: Where is the dye escaping? Where are vessels blocked?
- OCTA shows you the tiny vessels: Are capillaries gone? Are new ones growing?
What’s Changing Right Now
The biggest shift is the rise of wide-field OCTA. Older systems only captured the central retina. Now, newer machines can stitch together images of the entire retina - even the far edges. That’s huge. Many vascular problems start peripherally. If you only look at the center, you’re blind to early warning signs. Swept-source OCT is also becoming more common. It’s better at imaging through cataracts and seeing the choroid. That’s important for patients over 60 who often have both macular degeneration and cataracts. AI is starting to help too. Some clinics now use software that automatically measures retinal thickness or counts capillaries. It’s not replacing doctors - but it’s making measurements faster and more consistent.What You Should Know
If you’re being tested:- OCT is painless and quick - just sit still while the machine scans your eye.
- Fundus photos are bright but harmless. You might see spots afterward.
- Fluorescein angiography involves a needle. Your skin might turn yellow for a few hours. Your urine will be orange for a day.
- OCTA is like OCT - no injection, no discomfort.
Is OCT better than a regular eye exam?
A regular eye exam checks your vision and looks at the front of your eye. OCT looks deep into the retina - it’s not a replacement, it’s an upgrade. If you have diabetes, glaucoma, or macular degeneration, OCT gives information a regular exam can’t.
Does fluorescein angiography hurt?
The injection feels like a quick pinch, similar to a blood draw. Some people feel nauseous or warm afterward. The dye makes your skin and urine turn yellow or orange for up to 24 hours. Serious reactions are rare - under 1 in 10,000.
Can OCT detect glaucoma?
Yes. OCT measures the thickness of the nerve fiber layer around the optic nerve. Thinning here is one of the earliest signs of glaucoma - often before vision loss happens. It’s now a standard part of glaucoma monitoring.
Why do I need both OCT and OCTA?
OCT shows structure - fluid, thickness, layers. OCTA shows blood flow - capillaries, blockages, new vessels. You need both to understand if a problem is structural or vascular. For example, fluid in the retina could be from swelling (OCT) or from leaking vessels (OCTA).
Are these tests covered by insurance?
Most insurance plans, including Medicare, cover OCT, fundus photos, and fluorescein angiography when medically necessary - like for diabetes, macular degeneration, or retinal disease. OCTA is increasingly covered, but check with your provider. It’s often billed separately.
How often do I need these tests?
It depends on your condition. For stable macular degeneration, once a year. For active diabetic retinopathy, every 3-6 months. If you’re on treatment, your doctor will adjust based on what the images show. Don’t skip them - even if your vision feels fine.

Saylor Frye
January 4, 2026 AT 19:09OCTA is basically the Tesla of ophthalmic imaging - no dye, no hassle, just pure digital magic. The fact that we can now map capillary networks in 3D without poking a vein? That’s not progress, that’s a revolution. And yet, half the clinics still cling to FA like it’s 2008. I’ve seen residents get confused because their attending still thinks FA is the ‘gold standard’ - it’s not. It’s a relic with side effects.
SS-OCT with wide-field capability? That’s the real MVP. I had a patient last month with peripheral retinal ischemia - fundus photos were clean, OCT showed nothing, but wide-field OCTA revealed a whole network of non-perfused capillaries in the far periphery. If we hadn’t had that tech, she’d have been told she was ‘fine’ - and lost half her vision by next year.
AI-assisted thickness measurements? Yes. But don’t let the algorithm decide your treatment. I’ve seen AI miss subtle choroidal thinning because it was trained on old datasets. Human eyes still matter. Just… use the tools.
Also, stop calling OCT a ‘regular eye exam upgrade.’ It’s not an upgrade. It’s a different dimension. Like comparing a flashlight to a CT scan. One tells you if the room is dark. The other tells you where the pipes are leaking.
And yes, insurance covers it. If your doc says ‘it’s not necessary,’ ask them if they’d refuse an MRI for your knee because ‘it’s expensive.’
Kiran Plaha
January 5, 2026 AT 10:15This is very interesting. I never knew so much was happening inside the eye. I think doctors should explain this better to patients. My uncle had diabetes and he didn’t understand why they needed so many tests. He thought it was just to spend more money. But now I see - it’s not about money, it’s about seeing what we can’t see with our eyes.
Thank you for writing this. I will tell my family about it.
Isaac Jules
January 6, 2026 AT 12:48LMAO at all these people acting like OCTA is some futuristic miracle. It’s a glorified motion detector with zero sensitivity to leakage. You’re telling me we’re abandoning FA because it’s ‘invasive’? Bro, the dye is 99% safe. The real risk is misdiagnosing because you’re too lazy to use the right tool.
And don’t get me started on ‘AI-assisted measurements.’ You think a neural net trained on 10k scans can catch a tiny choroidal neovascularization hiding under drusen? No. It’ll say ‘normal’ and you’ll miss the lesion that costs someone their vision.
Stop marketing tech as ‘revolutionary’ when it’s just a partial solution. FA still catches what OCTA misses. Period. End of discussion. If your clinic doesn’t have FA, you’re cutting corners. And if you’re a patient - demand it.
Amy Le
January 8, 2026 AT 08:14Wow. I just realized how much we’ve lost by letting Big Pharma control what imaging tech gets funded. Why is OCTA still not standard everywhere? Because it doesn’t generate repeat revenue like FA does - you need dye every time, and that’s a profit center. But OCTA? One machine, infinite scans. No more dye sales.
So who’s stopping it? Not doctors. Not patients. Corporations. The same ones who delayed mammograms for Black women. The same ones who told us statins were ‘enough’ for heart disease while ignoring inflammation markers.
We’re not just talking about eye scans here. We’re talking about systemic medical neglect disguised as ‘innovation.’
And if your insurance won’t cover OCTA? Fight them. Your vision is not a commodity. 🇺🇸
Pavan Vora
January 9, 2026 AT 20:47Very informative, but I must say, I am confused about one thing - in India, most eye clinics still use old fundus cameras, and OCT is only available in big cities. And FA? Only in super-specialty hospitals. So when we talk about ‘wide-field OCTA’ and ‘swept-source OCT,’ it feels like we’re talking about a future that hasn’t reached us yet.
My cousin in Jaipur had diabetic retinopathy - they did fundus photo, and then said ‘come back in 6 months.’ No OCT, no angiography. How do we push for better access? Is there a movement? Or are we just waiting for the tech to trickle down?
Also, typo: ‘choriodal’ should be ‘choroidal’ 😅
Indra Triawan
January 10, 2026 AT 15:31I cried reading this. Not because I’m emotional - but because I remember my mother’s eyes. She was told ‘nothing’s wrong’ for two years while her vision faded. Then one day, someone did an OCT - and there it was. Fluid everywhere. Like a sponge soaked in water. They said, ‘If we’d caught this earlier…’
Why do we wait until it’s too late? Why is early detection still a luxury? I wish everyone could see what’s inside their eyes before they lose it. I wish I could show this to every doctor who said ‘it’s just aging.’
Thank you for writing this. I’m sharing it with everyone I know.
Harshit Kansal
January 12, 2026 AT 14:24Man, I had FA last year and I swear I felt like I was in a sci-fi movie - yellow vision, weird taste in my mouth, and then my pee turned orange for a whole day 😂
But honestly? Worth it. Found a leak I didn’t even know about. OCTA is wild though - no needle, just sit there and blink. My eye doc said it’s like a movie of my blood flow. I was like ‘wait, I can SEE my capillaries?’
Also, if you’re on insulin - get OCT yearly. No excuses. Your eyes don’t care if you’re ‘too busy.’
Brian Anaz
January 12, 2026 AT 18:11Let’s cut the crap. The U.S. has the best eye tech in the world. But half the population can’t access it because they don’t have insurance or live in a rural area. Meanwhile, China’s rolling out AI-powered OCT scanners in every village clinic. We’re sitting here debating whether OCTA is ‘better’ than FA while other countries are solving access.
This isn’t about tech superiority - it’s about equity. And if you’re not talking about that, you’re missing the point.
Also, FA isn’t ‘dangerous.’ It’s a 1 in 10,000 risk. But skipping it because you’re scared? That’s a 1 in 3 chance of going blind. Do the math.
Venkataramanan Viswanathan
January 14, 2026 AT 15:41It is with profound appreciation that I acknowledge the meticulous exposition provided herein regarding the modalities of retinal imaging. The delineation between structural and vascular assessment is not merely technical, but profoundly clinical in its implications.
One must, however, observe that the proliferation of OCTA, while undeniably advantageous, must be contextualized within the broader framework of diagnostic triage. The absence of dye-based angiography does not obviate the necessity of its judicious application in cases wherein leakage, rather than perfusion, constitutes the primary pathological concern.
Moreover, the integration of artificial intelligence into quantitative retinal analysis remains, at present, a supplementary instrument - not a replacement - for the seasoned ophthalmologist’s discernment.
May this discourse inspire equitable dissemination of these technologies, not merely as instruments of privilege, but as pillars of public health.
Vinayak Naik
January 15, 2026 AT 12:52Bro, OCTA is the real MVP. I work in a clinic and we just got our new SS-OCT with wide-field. We did a scan on this old guy who thought he was ‘fine’ - turned out he had a whole mess of weird vessels under his retina that no one saw before. We called it ‘spiderweb chaos’ 😆
And yeah, FA still has its place - like when the OCTA looks weird and you gotta confirm. But 80% of the time? We skip the needle now. Patient screams less, we get cleaner images, and no one’s skin turns yellow.
Also, AI’s getting scarily good at spotting early glaucoma. Last week it flagged a patient with 10% nerve thinning - doc said ‘I didn’t even notice.’ Now he’s on meds. Saved his sight.
TL;DR: Stop using 2010 tech when 2024 is right here. 🚀
Kelly Beck
January 16, 2026 AT 23:33You know what’s beautiful about this? It’s not just about the machines - it’s about the people behind them. The tech is amazing, but it’s the doctors who take the time to explain it, who don’t rush, who say ‘let’s look deeper’ - that’s what saves sight.
I used to think eye exams were just for glasses. Now I know they’re like a window into your whole body. Diabetes shows up here. High blood pressure shows up here. Even some brain issues can show in the retina.
So if you’re reading this and you’re scared of a test - don’t be. Ask questions. Demand the full picture. Your eyes are telling you stories. Don’t let them whisper forever.
You’re not just getting a scan - you’re getting a chance. And that’s worth every second. 💙👁️