When you’re managing type 2 diabetes, the last thing you want is for your medication to put you in the hospital-let alone risk your life. But between 2013 and 2018, the FDA documented 12 cases of a rare, deadly infection called Fournier’s gangrene linked to a common class of diabetes drugs: SGLT-2 inhibitors. These include Invokana, Farxiga, Jardiance, and Steglatro. The infection doesn’t just appear out of nowhere. It builds silently, then explodes-often in people who thought they were doing everything right.
What Is Fournier’s Gangrene?
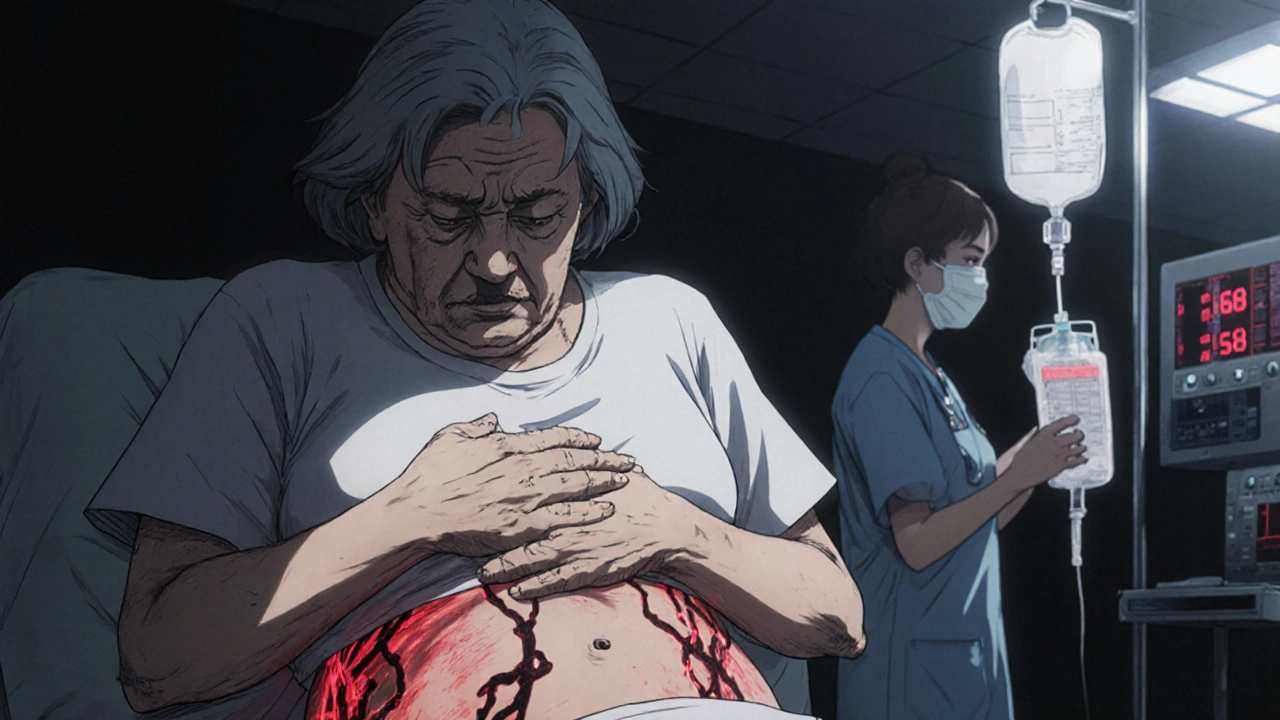
Fournier’s gangrene is a fast-moving bacterial infection that eats away at skin, fat, and muscle tissue in the genitals, perineum, or around the anus. It’s not a common condition-fewer than 1 in 10,000 people with diabetes will get it. But when it happens, it’s a medical emergency. Without surgery and strong antibiotics within hours, it can kill.
Before SGLT-2 inhibitors became popular, this condition mostly affected older men with diabetes, obesity, or weakened immune systems. But since 2018, cases have popped up in women, younger patients, and people with no obvious risk factors-except one: they were taking an SGLT-2 inhibitor.
How Do Diabetes Medications Cause This?
SGLT-2 inhibitors work by making your kidneys flush out extra sugar through urine. That lowers blood sugar-which is good. But that sugar doesn’t just disappear. It stays in your genital area, creating a sweet, moist environment where bacteria and yeast thrive. This is why so many people on these drugs get yeast infections or urinary tract infections. For most, it’s annoying but harmless.
But in rare cases, those infections don’t stay local. Bacteria can sneak through tiny tears in the skin or mucous membranes, then spread rapidly under the surface. Once they hit the fascia-the connective tissue beneath the skin-they start destroying everything in their path. The infection spreads faster than antibiotics can reach it. That’s why pain, swelling, and fever are warning signs you can’t ignore.
The Red Flags: Emergency Signs You Must Act On
If you’re taking one of these diabetes medications, know these symptoms. They’re not suggestions-they’re alarms.
- Severe pain or tenderness in your genitals, anus, or inner thighs-even if the area doesn’t look badly swollen yet
- Redness or swelling that spreads quickly, sometimes overnight
- Fever over 101°F (38.3°C) with chills or feeling extremely unwell
- Foul-smelling discharge from the genital or anal area
- Skin that feels warm, spongy, or crackles when touched (a sign of gas-producing bacteria)
- Pain that feels worse than it looks-this is a classic red flag in necrotizing infections
One woman, 71, on dapagliflozin, noticed a large abscess and foul odor near her anus. By the time she got to the ER, the infection had already eaten through layers of tissue. She needed multiple surgeries and weeks in the ICU. She survived. Others didn’t.

Who’s at Risk?
It’s not just men. The FDA and European regulators confirmed that about one-third of reported cases are in women. That’s a huge shift from the past, when Fournier’s gangrene was almost exclusively a male condition.
High-risk groups include:
- People with diabetes (especially if blood sugar is poorly controlled)
- Those who are overweight or obese (BMI over 30)
- Patients over 65
- Anyone with a history of genital infections while on SGLT-2 inhibitors
- People with weakened immune systems or recent trauma to the genital area
Even if you’re young and healthy, if you’re on one of these drugs and you notice any of the symptoms above-don’t wait. Don’t assume it’s just a yeast infection. Don’t wait until morning. Go to the ER now.
What Happens If You’re Diagnosed?
If a doctor suspects Fournier’s gangrene, they won’t wait for test results. They’ll start treatment immediately:
- Stop the SGLT-2 inhibitor-right away. No exceptions.
- IV antibiotics-usually a mix of drugs to cover multiple types of bacteria
- Emergency surgery to cut out dead tissue. Many patients need multiple surgeries over days or weeks
- ICU care-over 78% of reported cases required intensive care
According to a 2019 study of 19 cases, 15 patients needed ICU care. Twelve needed more than one surgery. Three died. Even with the best care, this infection kills up to 20% of the time.
Are These Drugs Still Safe to Use?
Yes-but with serious caveats.
The FDA, Health Canada, the European Medicines Agency, and Medsafe in New Zealand all agree: the benefits of SGLT-2 inhibitors still outweigh the risks-for most people. These drugs don’t just lower blood sugar. They reduce heart failure hospitalizations, lower the risk of kidney failure, and even cut the chance of dying from heart disease.
But that doesn’t mean they’re risk-free. If you’ve had recurrent yeast infections or UTIs while on these drugs, talk to your doctor. There are other diabetes medications without this risk. Metformin, GLP-1 agonists like semaglutide, and insulin don’t carry the same danger.
The key is awareness. If you’re on an SGLT-2 inhibitor, your doctor should have warned you about these signs. If they didn’t, ask. And if you’re experiencing any of the symptoms listed above-go to the ER. Don’t call your doctor first. Don’t wait. This isn’t something you can treat at home.
What Should You Do Now?
If you’re taking one of these medications:
- Know the symptoms. Print them out. Put them on your fridge.
- Check your genital area daily, especially if you’re prone to infections.
- If you notice swelling, pain, or odor-go to the ER immediately. Tell them you’re on an SGLT-2 inhibitor.
- Ask your doctor if you’re a good candidate to switch to a different diabetes drug.
- Don’t stop the medication on your own. But don’t ignore symptoms either.
Diabetes management is a balancing act. You need to control your blood sugar without trading one danger for another. Fournier’s gangrene is rare-but when it strikes, it doesn’t give you time to think. Your best defense is knowing what to look for-and acting before it’s too late.

Monica Lindsey
December 1, 2025 AT 08:37So let me get this straight-you’re telling me people are dying because they took a drug that makes them pee out sugar? And now we’re supposed to be surprised? If you can’t control your blood sugar without turning your genitals into a yeast farm, maybe you shouldn’t be on a drug that turns your body into a petri dish.
jamie sigler
December 1, 2025 AT 23:26I mean... I guess I should’ve seen this coming. My doctor just handed me a prescription like it was a coupon for free coffee. No warning. No ‘this might eat your junk off.’ Now I’m just mad I didn’t ask more questions.
Peter Lubem Ause
December 2, 2025 AT 09:11This is one of those rare cases where modern medicine’s brilliance comes with a terrifying side effect. SGLT-2 inhibitors are revolutionary-they save hearts, protect kidneys, reduce mortality. But biology doesn’t care about our good intentions. Sugar in urine? It’s like leaving a buffet out in the jungle and wondering why the lions showed up. The body isn’t broken when this happens-it’s just being exploited by a pathogen that evolved to thrive where we didn’t expect it. This isn’t negligence. It’s unintended consequence. But awareness? That’s the real medicine here. If you’re on one of these drugs, don’t wait for the pain to be ‘bad enough.’ If your skin feels warm and spongy, or you smell something rotten near your groin-go to the ER. Not tomorrow. Not after work. Now. Your life isn’t a waiting room.
linda wood
December 3, 2025 AT 10:37Oh wow, so the drug that’s supposed to help me live longer might also make me die screaming from a rotting crotch? Thanks, Big Pharma. Really thought I was being proactive by taking my pills.
gerardo beaudoin
December 4, 2025 AT 05:57Yeah, this is wild. I’ve been on Jardiance for two years and never thought twice about UTIs. Now I’m checking myself in the mirror every morning like I’m auditioning for a horror movie. But honestly? Better safe than sorry. I’m gonna ask my doc about switching.
tushar makwana
December 5, 2025 AT 02:16in india we dont hear much about this but my uncle had diabetes and he got some kind of infection near his private part, he was in hospital for weeks. i think this is global problem not just usa thing. people need to know.
Richard Thomas
December 5, 2025 AT 05:45It is imperative to underscore that the pharmacokinetic profile of SGLT-2 inhibitors, while efficacious in reducing glycated hemoglobin, inadvertently fosters a microenvironment conducive to the proliferation of facultative anaerobes in the perineal region. The resultant necrotizing fasciitis, though statistically rare, constitutes a paradigmatic example of iatrogenic pathology requiring immediate surgical intervention and multidisciplinary critical care. Regulatory agencies have appropriately revised labeling protocols, yet public awareness remains woefully inadequate. The onus lies not solely with clinicians, but with the patient population to recognize the prodromal signs-particularly cutaneous crepitus and disproportionate pain-which are pathognomonic and demand emergency triage.
Sara Shumaker
December 6, 2025 AT 19:31It’s strange how we treat diabetes like a puzzle with one perfect solution. We chase the lowest A1c, the most ‘advanced’ drugs, the newest pills-like the body is a machine we can optimize without consequences. But life isn’t an algorithm. This infection? It’s not a bug. It’s a whisper from our biology saying, ‘You’re forcing me to adapt in ways I wasn’t meant to.’ Maybe the real question isn’t whether these drugs are safe-but whether we’re asking too much of our bodies in the name of control.
Scott Collard
December 7, 2025 AT 04:14You’re all overreacting. If you’re worried about your junk rotting, maybe don’t take the drug. Simple. Stop whining.
Robert Bashaw
December 7, 2025 AT 13:49My cousin’s ex-husband got this thing. They said his balls looked like a deflated balloon full of rotten meat. He screamed for three days before they cut off half his pelvis. Now he walks with a cane and cries during sex. This isn’t a side effect-it’s a horror movie sequel no one asked for.
Brandy Johnson
December 9, 2025 AT 04:01It’s unacceptable that American pharmaceutical companies prioritize profit margins over patient safety. This is yet another example of regulatory capture and corporate negligence. The FDA’s response was tepid. We need class-action lawsuits, mandatory black-box warnings, and public shaming of executives who knew and did nothing.