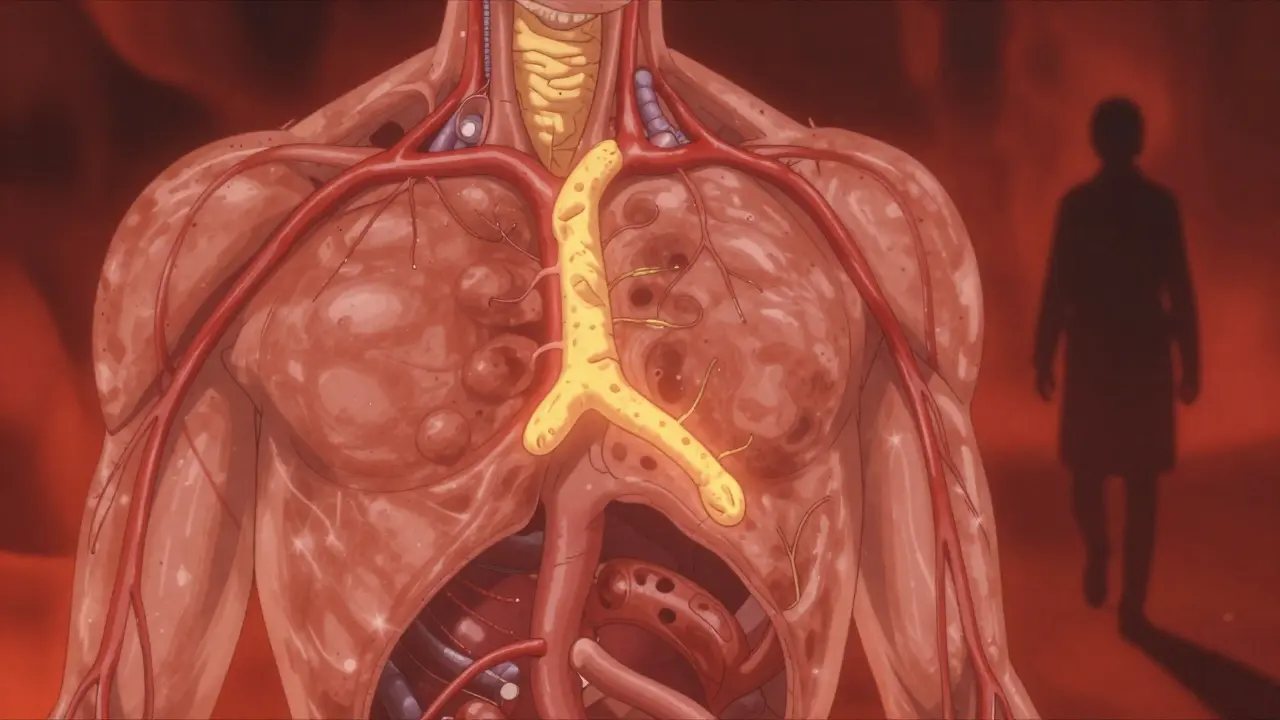
Most people don’t feel high cholesterol until it’s too late. There’s no pain, no warning sign, no sudden dizziness. Just silent buildup-fatty deposits creeping through your arteries, slowly narrowing the path for blood to reach your heart and brain. By the time symptoms show up, it’s often because a clot has formed, or an artery is already blocked. That’s why knowing about hypercholesterolemia isn’t just helpful-it’s life-saving.
What Exactly Is Hypercholesterolemia?
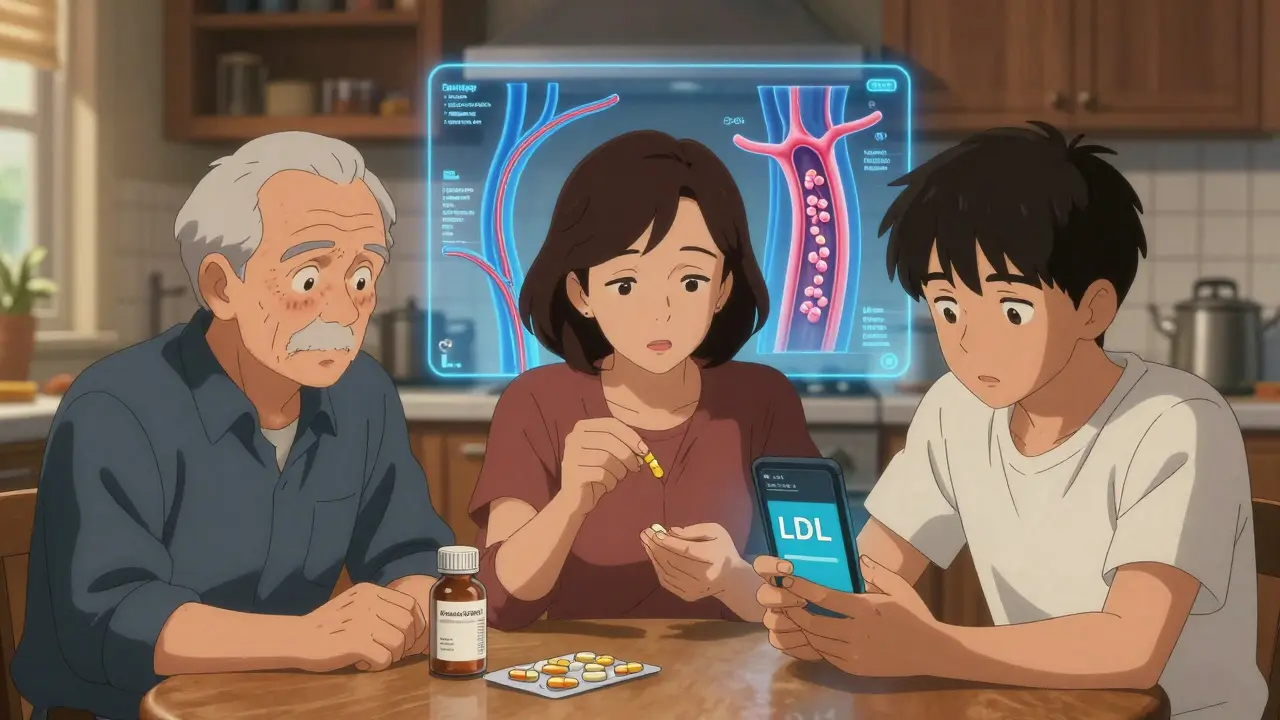
Hypercholesterolemia means your blood has too much cholesterol. Cholesterol itself isn’t bad. Your body needs it to build cells, make hormones, and digest food. But when levels get too high-especially the kind called LDL, or "bad" cholesterol-it starts sticking to artery walls. Over time, that builds up into plaque. Plaque hardens, narrows arteries, and can break off to trigger a heart attack or stroke.
The numbers matter. The American Heart Association says total cholesterol above 200 mg/dL is considered elevated. But what really counts is your LDL level. If it’s above 190 mg/dL, that’s classified as severe hypercholesterolemia. Even levels between 130 and 159 mg/dL can be dangerous if you have other risk factors like high blood pressure, diabetes, or a family history of early heart disease.
Familial vs. Acquired: Two Very Different Causes
Not all high cholesterol is the same. There are two main types: genetic (familial) and lifestyle-related (acquired).
Familial hypercholesterolemia (FH) is inherited. One faulty gene from a parent can send LDL levels soaring from birth. About 1 in 250 people have this condition, but most don’t know it. People with heterozygous FH-meaning they got the gene from one parent-often have LDL levels between 190 and 400 mg/dL. Those with homozygous FH, who got it from both parents, can have levels over 450 mg/dL. These individuals are at extreme risk: untreated, they can have heart attacks before age 20.
Physical signs can hint at FH. Yellowish fatty deposits around the eyelids (xanthelasmas) or thickened tendons in the heels or knuckles (tendon xanthomas) are telltale markers. If you or a close relative has these, get tested-even if you’re young.
Acquired hypercholesterolemia, on the other hand, comes from what you eat, how active you are, or other health problems. Poor diet, lack of exercise, obesity, smoking, and excessive alcohol all contribute. Medical conditions like hypothyroidism, chronic kidney disease, and type 2 diabetes also raise cholesterol. Some medications, like certain diuretics or steroids, can nudge levels up too.
Why It’s Silent-And Why That’s Dangerous
Dr. Roger Blumenthal from Johns Hopkins puts it bluntly: "High cholesterol is a silent killer." You won’t feel it until your arteries are 70% blocked. That’s why routine screening is non-negotiable. The U.S. Preventive Services Task Force recommends a lipid panel for all adults between 40 and 75. But if you have a family history of early heart disease, or if you’re overweight or diabetic, you should get tested even earlier-even in your 20s.
And here’s something many don’t realize: fasting isn’t required anymore for basic cholesterol tests. You can walk in, get blood drawn, and get results without skipping breakfast. That makes checking your numbers easier than ever.
How High Is Too High? The Numbers That Matter
Let’s break down what your numbers mean:
- Total cholesterol: Below 200 mg/dL is ideal. 200-239 is borderline high. 240+ is high.
- LDL (bad cholesterol): Below 100 mg/dL is optimal. 100-129 is near optimal. 130-159 is borderline high. 160-189 is high. 190+ is very high.
- HDL (good cholesterol): Above 60 mg/dL is protective. Below 40 for men or 50 for women is a risk factor.
- Triglycerides: Below 150 mg/dL is normal. Above 200 is high.
These aren’t just numbers on a page. For every 39 mg/dL drop in LDL, your risk of a heart attack or stroke drops by 22%. That’s the power of lowering cholesterol.
How Is It Treated? From Diet to Drugs
First step: lifestyle changes. For many, especially those with acquired hypercholesterolemia, diet and exercise alone can cut LDL by 10-15%. The Portfolio Diet-rich in plant sterols, oats, nuts, soy, and fiber-has been shown in clinical trials to reduce LDL by nearly 30%. But sticking to it is hard. Only about half of people keep it up past a year.
If lifestyle isn’t enough, medication kicks in. Statins are the first-line treatment. Drugs like atorvastatin and rosuvastatin can slash LDL by 50% or more. They’re safe, well-studied, and proven to save lives. But some people can’t tolerate them-about 7-29% experience muscle pain or other side effects.
For those people, or for those with FH, other options exist:
- Ezetimibe: Blocks cholesterol absorption in the gut. Lowers LDL by about 18%.
- PCSK9 inhibitors: Injectable drugs like alirocumab and evolocumab. They can drop LDL by another 50-60% on top of statins.
- Inclisiran (Leqvio): A newer shot given just twice a year. It works at the genetic level to reduce LDL production. A game-changer for adherence.
People with FH often need all three: a high-dose statin, ezetimibe, and a PCSK9 inhibitor. That’s not over-treatment-it’s survival.
Why So Many People Aren’t Getting Help
Here’s the ugly truth: even though we have effective treatments, most people with high cholesterol aren’t getting them. In the U.S., only 55.5% of adults who should be on statins are actually taking them. Among Black adults, the rate drops to 42.3%. Women are less likely to be prescribed statins than men, even when their risk is the same.
Why? A mix of things. Some don’t know they have it. Others don’t feel sick, so they skip meds. Some worry about side effects. Others can’t afford them-even though many generics cost less than $10 a month.
And the cost of doing nothing? The American Heart Association estimates cholesterol-related heart disease costs the U.S. $218 billion a year. That’s $142 billion in medical bills and $76 billion lost to missed work and early death.
What’s New? The Future of Cholesterol Management
The field is moving fast. Genetic testing is becoming more accessible. Polygenic risk scores can now identify people who have high cholesterol not from one gene, but from dozens of small genetic tweaks-people who might need earlier intervention than we used to think.
Also, tools like digital reminders, apps that track diet and meds, and telehealth follow-ups are helping people stick to treatment. And new guidelines are clearer: for very high-risk patients, doctors are now aiming for LDL below 55 mg/dL-not just "lowering it by 50%".
The big challenge ahead? Obesity. As more people become overweight or obese, secondary hypercholesterolemia is rising. By 2030, half of U.S. adults could be obese. That means more diabetes, more inflammation, more clogged arteries.
What You Can Do Right Now
You don’t need a PhD to take control. Here’s what works:
- Get tested. If you’re 40 or older, ask for a lipid panel. If you have risk factors, get tested sooner.
- Know your numbers. Write them down. Understand what LDL means for you.
- Move more. Even 30 minutes of brisk walking five days a week helps.
- Eat smarter. Swap butter for olive oil. Choose whole grains over white bread. Add beans, oats, nuts, and fatty fish to your meals.
- Talk to your doctor. If your LDL is high, don’t wait. Ask about statins. Ask about other options. Don’t assume you can "just eat better."
High cholesterol isn’t your fault. But managing it? That’s your power. You can’t change your genes. But you can change your next blood test. And that’s enough to keep you alive longer, healthier, and free from the fear of a heart attack.
Can high cholesterol run in families?
Yes. Familial hypercholesterolemia (FH) is a genetic condition passed down from parent to child. If one parent has it, each child has a 50% chance of inheriting it. People with FH have very high LDL from birth and are at serious risk for early heart disease. Even if you feel fine, if close relatives had heart attacks before age 55 (men) or 65 (women), you should get tested.
Do I need to fast before a cholesterol test?
No, not anymore. For most standard lipid panels, fasting isn’t required. You can eat and drink normally before your blood draw. This makes testing more convenient and increases the chance people will actually get checked. However, if your doctor orders a full lipid panel that includes triglycerides, they may still ask you to fast for 9-12 hours-so always check with your provider.
Are statins safe for long-term use?
Yes. Statins have been used for over 30 years and studied in millions of people. The benefits far outweigh the risks for most. Side effects like muscle pain occur in only 7-29% of users, and often go away with dose adjustments or switching medications. Serious side effects like liver damage or muscle breakdown are extremely rare. The real danger isn’t taking statins-it’s ignoring high cholesterol and risking a heart attack.
Can I lower cholesterol without medication?
For some people, yes-especially if high cholesterol is caused by diet, weight, or inactivity. The Portfolio Diet (oats, nuts, plant sterols, soy, fiber) can lower LDL by up to 30%. Losing 5-10% of body weight can also make a big difference. But if you have familial hypercholesterolemia or already have heart disease, lifestyle alone won’t be enough. Medication is necessary to reach safe LDL levels.
Is dietary cholesterol still a concern?
The science has shifted. While eggs and shellfish contain cholesterol, research now shows that saturated and trans fats have a much bigger impact on blood cholesterol levels. The Dietary Guidelines no longer set a daily limit for dietary cholesterol. But a 2019 JAMA study found that each extra 300 mg of dietary cholesterol per day (about one and a half eggs) was linked to a 17% higher risk of heart disease. So moderation still matters-especially if you’re already at risk.
How often should I get my cholesterol checked?
If you’re 40-75 and have no known heart disease or risk factors, get tested every 4-6 years. If you’re younger but have obesity, diabetes, high blood pressure, or a family history of early heart disease, get tested every 1-2 years. If you’re on medication, your doctor will check your levels every 3-12 months to make sure it’s working.

Herman Rousseau
December 21, 2025 AT 13:31Just got my lipid panel back - LDL at 198. Felt like a punch in the gut. But hey, I’m 38, active, eat mostly plants, and still got hit with this? Turns out my dad had a heart attack at 47. 🤯 Time to get serious. Started statins this week. No more "I’ll eat better next month."
Johnnie R. Bailey
December 22, 2025 AT 19:16Cholesterol isn’t the villain - it’s the messenger. The real question isn’t "how low can we push LDL?" but "why is the body screaming this signal?" Inflammation, insulin resistance, oxidative stress - these are the true architects of plaque. We treat the symptom, not the symphony.
And yet - statins work. Not because they’re magic, but because they disrupt a cascade we still don’t fully understand. Sometimes fixing the symptom *is* saving the life.
Vikrant Sura
December 23, 2025 AT 15:00Another article telling people to take statins. Bro, just stop eating bread and sugar. Everyone’s obsessed with cholesterol like it’s the root of all evil. Meanwhile, your sugar intake is 80g a day and you’re shocked you have high LDL? 🙄
Ajay Brahmandam
December 25, 2025 AT 01:08My uncle had FH. LDL over 500. Didn’t know till he had a heart attack at 39. We all got tested. I had 210. Started on ezetimibe + low-dose statin. Lost 25 lbs. Walked 6k steps daily. Now my LDL is 82. No side effects. Just… consistent. Don’t overcomplicate it.
And yeah, fasting isn’t needed anymore. Thank god. I forgot I had an appointment last month and ate pancakes. Still got accurate results. 😅
Tarun Sharma
December 25, 2025 AT 11:37It is imperative that individuals undergo regular lipid profiling, particularly if familial predisposition is present. The clinical significance of LDL elevation cannot be overstated. Adherence to pharmacological intervention remains suboptimal across demographic strata, necessitating systemic healthcare reform.
Aliyu Sani
December 26, 2025 AT 09:25man… cholesterol ain’t just about diet. it’s like your body’s got a broken alarm system. you got genes throwin’ fire everywhere, and then you eat a fry and the whole house burns down. statins? yeah they work. but why we still treat the symptom and not the damn system? 🤔
also… who even knows what "polygenic risk score" means? sounds like sci-fi but it’s real. my cousin got tested, turns out she’s got 12 sneaky gene variants all whispering "heart attack soon". wild.
Gabriella da Silva Mendes
December 27, 2025 AT 23:23Okay but let’s be real - this whole "cholesterol is silent killer" thing is just Big Pharma’s way to sell more pills. I’m 42, eat avocado toast, drink green juice, and my doctor wants to put me on a statin because my LDL is 165? Nah. I’d rather just take turmeric and pray. 🙏
Also, why are women always last on the list? My brother got statins at 35, I’m 42 and they’re still "monitoring" me. Classic. 💅
Jim Brown
December 28, 2025 AT 03:50Cholesterol, as a molecule, is neither good nor evil. It is a structural imperative of cellular life. The moral panic surrounding it is a reflection of our cultural fear of bodily impermanence - we project onto lipid profiles our dread of mortality. Yet, the empirical data is unambiguous: lowering LDL reduces cardiovascular events, regardless of philosophical discomfort.
Perhaps the real disease is our refusal to accept that biology does not care for our narratives.
Sam Black
December 28, 2025 AT 07:25For anyone feeling overwhelmed - start small. Swap one processed snack for almonds. Walk after dinner. Talk to your doc about your family history. You don’t need to overhaul your life tomorrow. Just show up, one choice at a time.
Also - if you’re on a statin and feel weird? Tell your doctor. There are 5+ types. One might fit you like a glove. Don’t quit because one didn’t work. You’re not failing. The system just hasn’t found your fit yet.
Jamison Kissh
December 29, 2025 AT 06:20What’s wild is how we treat familial hypercholesterolemia like it’s a personal failure. Imagine if someone had a genetic disease causing blindness - we wouldn’t say "just eat less light." Why do we do this with cholesterol?
And yet - we still don’t screen teens. Why? Because it’s "rare"? 1 in 250 isn’t rare. It’s a public health blind spot. We need mandatory pediatric lipid panels. Like vaccines.
Tony Du bled
December 29, 2025 AT 12:57My grandma had xanthomas. Yellow bumps on her eyelids. We thought it was just "old age." Turns out she had homozygous FH. Died at 52. My dad got tested - same thing. Now my 12-year-old nephew is on a statin. He doesn’t even know what cholesterol is. But his arteries do.
It’s not a lifestyle disease for some of us. It’s a family curse. And we’re just now learning how to fight it.
Art Van Gelder
December 30, 2025 AT 22:22Let me tell you about my friend’s sister - she’s 31, vegan, yoga instructor, drinks kale smoothies every morning. Her LDL? 214. She cried for a week. Turns out - she’s got the gene. All the "eat clean" in the world won’t fix that. She’s now on a PCSK9 inhibitor. $14,000 a year. Insurance covers it. But what about the person who can’t afford it? What about the uninsured? This isn’t just medicine - it’s a class issue wrapped in a blood test.
And don’t get me started on how the medical system treats women’s symptoms as "anxiety" until it’s too late. I’ve seen it. Too many times.
Kathryn Weymouth
January 1, 2026 AT 07:19Regarding dietary cholesterol: the 2019 JAMA study you referenced had significant limitations - it was observational, self-reported, and didn’t control for overall dietary patterns. A single egg per day is not equivalent to a daily bacon-egg-cheese sandwich with white toast and syrup. Context matters. Don’t demonize whole foods based on isolated data points.
Nader Bsyouni
January 1, 2026 AT 09:30statins are a scam the medical industrial complex sells to keep you dependent and broke. your body makes cholesterol because it needs it. if you lower it too much you get depression and brain fog. the real killer is sugar and processed carbs not cholesterol. also why are you all so obsessed with numbers? life is not a lab report. just live. breathe. eat real food. stop listening to doctors who make money off your fear