Missing a dose of your medication happens to almost everyone at some point. Maybe you slept through your alarm. Maybe you were rushing out the door. Maybe you forgot because you’re juggling five different pills. The instinct is clear: take two now to make up for it. But that’s exactly what you should not do. Doubling up can land you in the emergency room - and it’s more common than you think.
In England alone, taking double doses accounts for 14.2% of preventable hospital admissions tied to medication errors. That’s nearly 1 in 7 cases. The cost? Over £98 million a year to the NHS. And it’s not just about money. For drugs like warfarin, digoxin, or methotrexate, doubling a dose can trigger internal bleeding, heart rhythm problems, or organ failure. You don’t need to panic - you just need to know what to do instead.
Why Doubling Up Is Dangerous
Medications aren’t like coffee. If you skip your morning cup, you can have two later and feel fine. Drugs work differently. They’re designed to stay in your system at a steady level. Too much at once? That’s a spike. And for some medicines, even a small spike can be deadly.
Take warfarin, a blood thinner. Its safe range is razor-thin: 0.5 to 0.9 ng/mL in your blood. Go above 5.0? Your risk of serious bleeding skyrockets. A 2022 Johns Hopkins study found that 68.4% of patients who doubled their warfarin dose ended up with INR levels over 5.0. That’s not a warning - that’s a red flag.
Same goes for methotrexate, used for autoimmune diseases and sometimes cancer. The NHS explicitly says: never take a double dose. One extra milligram can poison your bone marrow. Even common drugs like antibiotics or blood pressure pills can cause dizziness, nausea, or dangerously low heart rates if you double up.
The rule is simple: never take a double dose to make up for a missed one. This isn’t advice - it’s a safety standard backed by the FDA, NHS, MHRA, and every major medical body.
What to Do Instead: The Timing Rule
The real answer isn’t about taking more - it’s about timing. When you realize you missed a dose, ask yourself: How close am I to my next dose?
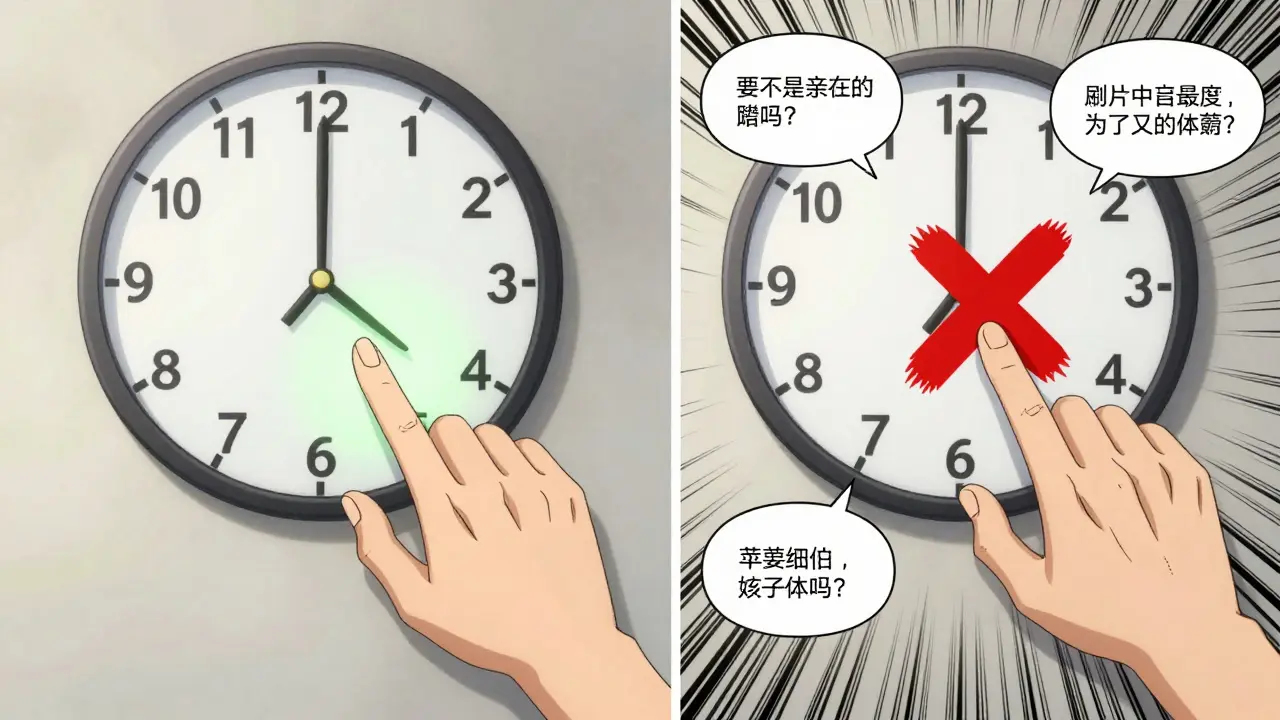
For most medications, the guideline is the midpoint rule. If you remember before halfway to your next scheduled dose, take it. If you’re past that point, skip it. No exceptions.
Let’s say you take a pill at 8 a.m. and 8 p.m. every day. Your midpoint is 2 p.m. If you remember at 1 p.m., take the missed dose. If it’s 3 p.m.? Skip it. Wait for your next dose at 8 p.m.
This works for most once-daily and twice-daily meds. But some drugs need special rules.
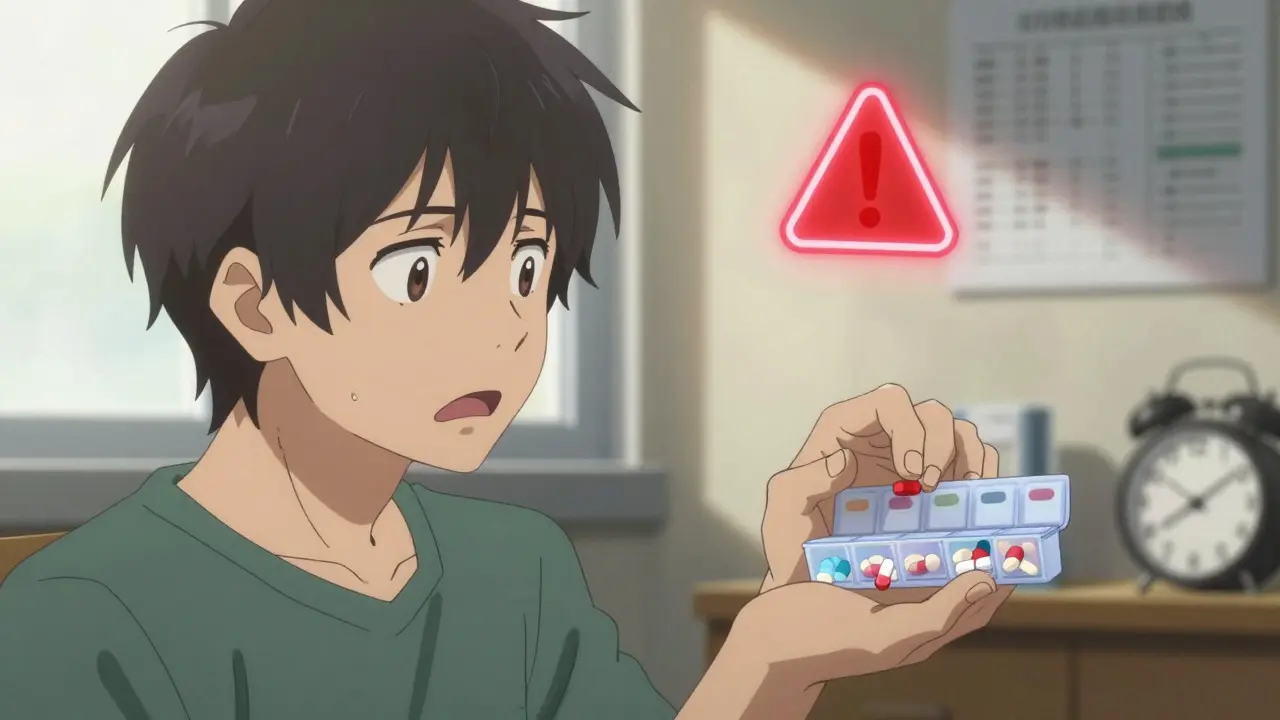
Special Cases: High-Risk Medications
Not all pills are created equal. Some have narrow therapeutic windows - meaning the difference between healing and harming is tiny. These are labeled as red risk by the National Patient Safety Agency. Examples: anticoagulants, antiepileptics, immunosuppressants, insulin, and digoxin.
Warfarin: If you miss your evening dose and remember before midnight, take it. If it’s after midnight? Skip it. Don’t take it the next morning - that would be two doses too close together.
Insulin: This one’s tricky. If you miss a mealtime insulin dose, don’t just inject it later. Blood sugar can crash or spike unpredictably. Call your doctor or pharmacist. They’ll tell you whether to adjust your next dose or monitor your glucose closely.
Antiepileptics: Missing even one dose can trigger a seizure. If you forget, take it as soon as you remember - but only if it’s within 4-6 hours of your usual time. After that, skip it. Never double up. The risk of seizures from missing a dose is far lower than the risk of toxicity from doubling.
Oral contraceptives: If you miss an active pill by less than 12 hours, take it right away. If it’s more than 12 hours late, take it when you remember - but use backup contraception (like condoms) for the next 7 days. Missing two pills in a row? Call your provider. You may need emergency contraception.
GLP-1 medications (like semaglutide or tirzepatide): You can take a missed dose up to 4 days late. But if you miss two doses in a row (14 days total), don’t just jump back in. Talk to your doctor. Resuming after a long break can cause nausea or vomiting in over 23% of patients.
What About Once-Daily Pills?
For once-daily medications - like statins, thyroid pills, or blood pressure meds - the rule is simple: take it if you remember on the same day. If you don’t remember until the next day? Skip it. Don’t take two the next day.
Levothyroxine (thyroid medication) is a common trap. Some patient leaflets wrongly say to take it immediately whenever you remember. That’s not right. Because it has a 7-day half-life, missing one day won’t hurt. But taking two doses together can cause heart palpitations or bone loss over time. Take it only if you remember before midnight. Otherwise, wait.
What About Twice-Daily or More?
Twice-daily meds (like metoprolol or amoxicillin) have a 6-hour window. If your dose is at 8 a.m. and 8 p.m., you can take a missed morning dose until 2 p.m. - then skip it. Same for the evening dose: take it until 2 a.m. the next day, then skip.
Some antibiotics, like amoxicillin, are exceptions. In rare cases, doubling the first missed dose is okay - but only if you haven’t taken any other doses since. This applies to less than 3% of all prescriptions. Don’t guess. Check your leaflet or call your pharmacist.
Why Do So Many People Get It Wrong?
It’s not your fault. A 2021 review found that 25% of high-risk medications have no missed dose instructions in their official patient leaflets. Even worse, 41.7% of those leaflets give conflicting advice.
Patients often think: If I miss a dose, I need to catch up. But clinicians know better. In one study, 53% of doctors recommended taking the dose if within a safe window - but only 22% of patients knew that. That gap is dangerous.
And it’s not just confusion. One patient in Toronto told me she got three different answers from three different pharmacies about her blood pressure pills. That’s not a fluke. It’s systemic.
Tools to Help You Stay on Track
You don’t have to rely on memory. Digital tools work. A 2023 study showed MyTherapy app users reduced missed doses by 42.3%. Simple alarms on your phone help too. Set two: one for the morning, one for the evening. Label them with the pill name.
Pharmacies in Canada and the UK now offer free Medicines Use Reviews. A pharmacist sits with you, checks all your meds, and draws up a clear missed-dose plan. In one King’s Fund study, this cut missed doses by nearly 28%.
And if you’re traveling across time zones? Set your phone alarms to your home time - not local time - until you’ve adjusted. A 2023 survey found that 38.7% of travelers made medication errors because they switched clocks too soon.
When to Call for Help
You don’t need to figure this out alone. Call your pharmacist if:
- You missed a dose of a high-risk medication (warfarin, insulin, antiepileptic, methotrexate)
- You’re not sure about the timing rule
- You took a double dose by accident
- You’ve missed two or more doses in a row
For emergencies - like chest pain, trouble breathing, or uncontrolled bleeding - go to the ER. But if you’re just unsure? Call your pharmacy. They’re trained for this.
The MHRA’s Yellow Card system lets you report medication errors anonymously. If your pill’s instructions are unclear, report it. That’s how standards get better.
The Bigger Picture
Every year, 237 million doses are missed in UK hospitals alone. That’s not just about patients forgetting. It’s about systems failing. New rules are coming. By 2025, all new drugs in Europe must include evidence-based missed-dose instructions. That’s progress.
But until then, you’re your own best advocate. Know your meds. Know your timing. And never, ever double up.
What should I do if I accidentally took a double dose?
If you took a double dose by accident, stay calm. Don’t take any more pills. Call your pharmacist or poison control immediately. For high-risk drugs like warfarin, insulin, or methotrexate, go to the ER. For others, like blood pressure or cholesterol pills, monitor for symptoms like dizziness, nausea, or rapid heartbeat. Keep your pill bottles handy - the pharmacist will need to know exactly what you took and when.
Can I skip a dose if I’m feeling fine?
No. Feeling fine doesn’t mean your medication isn’t working. Many drugs, like blood pressure or thyroid pills, prevent problems before they start. Skipping doses - even when you feel good - can cause long-term damage. For example, missing one dose of warfarin might not cause bleeding right away, but over time, it raises your stroke risk. Stick to the schedule unless your doctor says otherwise.
Do all medications have the same missed-dose rules?
No. Rules vary by drug type, half-life, and risk level. High-risk drugs like anticoagulants or antiepileptics have strict skip-if-near-next-dose rules. Low-risk drugs like statins are more forgiving - missing one dose won’t hurt much. Always check your specific medication’s instructions. Don’t assume one rule fits all.
Is it safe to take a missed dose the next day?
Never take a missed dose the next day unless your doctor or pharmacist specifically says so. Taking a dose from the previous day with your current day’s dose means you’re doubling up. Even if you think you’re “just catching up,” you’re putting yourself at risk. Always take only your scheduled dose for that day.
How can I remember to take my pills every day?
Use a pill organizer with compartments for morning, afternoon, and night. Set phone alarms labeled with your pill names. Download a medication tracker app like MyTherapy. Ask a family member to check in with you. Talk to your pharmacist about a Medicines Use Review - they can simplify your routine and help you build a system that works for your life.
If you’re managing multiple medications, don’t wait for a crisis. Schedule a free Medicines Use Review with your local pharmacy. It takes 20 minutes - and it could save your life.

Jacob Hill
January 18, 2026 AT 21:10Wow, this is one of the clearest, most actionable guides I’ve ever read on medication safety-seriously, thank you for laying this out so precisely! The midpoint rule? Genius. I’ve been using it for my blood pressure meds since last year, and it’s cut my missed doses by half. Also, the warfarin INR stats? Chilling. I didn’t realize how razor-thin that window is.
Christi Steinbeck
January 19, 2026 AT 11:14THIS. I’ve been telling my mom for years not to double up on her pills-and now I can just send her this. She’s on five meds, and she always thinks skipping one means she’s ‘being good’ by not taking too much. This post is going in her folder. Seriously, thank you for writing this. We need more like it.
Phil Hillson
January 19, 2026 AT 23:48Look I get it but why does everything have to be so complicated? I just take my pills when I remember. If I miss one I take it next day. Done. Why are we turning simple things into medical horror stories? My grandma took warfarin for 20 years and never went to the ER. Maybe you guys just overthink everything
Josh Kenna
January 20, 2026 AT 05:22bro i just read this whole thing and i think you're right about the midpoint rule but i also think we need better packaging. like why do my pills not have a little sticker that says 'if you miss it after 2pm skip it'? i had to google this and now i feel dumb. also i took a double dose last week on accident and my heart felt weird for 2 hours. i'm scared now
Erwin Kodiat
January 21, 2026 AT 03:52Man, I used to be the guy who doubled up like it was a game of catch-up. Then I had a panic attack after accidentally taking two blood pressure pills. Never again. This post saved me from becoming a statistic. Seriously, thank you. I’ve started using MyTherapy and it’s weirdly satisfying to see the streaks grow. Small wins, y’know?
Aman Kumar
January 21, 2026 AT 05:30While the clinical guidelines presented are technically accurate, they reflect a Western biomedical hegemony that pathologizes human forgetfulness as a deficit rather than a systemic failure of pharmaceutical design. The very notion of a 'midpoint rule' assumes temporal discipline, which is inaccessible to those working multiple shifts, caring for children, or navigating linguistic barriers. The NHS spends £98 million to correct behaviors that are, in fact, rational adaptations to an incoherent medication regime. We must redesign the system-not shame the patient.
Valerie DeLoach
January 21, 2026 AT 09:34Aman, your point about systemic failure is critical-and I’d add that the lack of standardized, patient-friendly instructions is a form of medical negligence. The fact that 41.7% of leaflets give conflicting advice? That’s not an oversight. It’s negligence. We need mandatory, plain-language, multilingual, visual guides on every prescription bottle. No more ‘consult your doctor’ as a cop-out. Patients aren’t failing. The system is.
Lewis Yeaple
January 22, 2026 AT 06:32It is imperative to note that the midpoint rule, while widely disseminated, lacks formal endorsement by the American College of Clinical Pharmacy. The ACCP recommends adherence to the manufacturer’s labeled instructions, which vary by drug class and pharmacokinetic profile. The generalization presented herein may lead to unintended consequences, particularly in polypharmacy patients. One must consult the prescribing physician before implementing any heuristic.
sujit paul
January 23, 2026 AT 01:44Have you ever wondered why these rules are so strict? Who benefits? Pharmaceutical companies. They want you to take the exact dose at the exact time-because if you miss it, you might need another prescription. If you double up, you might go to the ER. And if you go to the ER, they bill your insurance. It’s a cycle. They profit from your confusion. Don’t be fooled.
Tracy Howard
January 25, 2026 AT 00:57Look, I’m Canadian, and I’ve seen this mess up close. The NHS is broke, so they offload the burden onto patients. Meanwhile, our pharmacists here do Medicines Use Reviews for free-no BS, no jargon, just someone sitting down with you and saying, ‘Here’s your chart, here’s what matters.’ Why can’t the U.S. do this? Because we’ve turned healthcare into a profit pipeline. We need to fix the system, not just teach people how to survive it.
Jake Rudin
January 26, 2026 AT 04:18There’s a deeper philosophical layer here: time itself has been medicalized. We’re no longer living by natural rhythms-we’re living by pill schedules. The body doesn’t care about 8 a.m. or 8 p.m. It cares about balance. The ‘midpoint rule’ is a crude approximation of a biological truth we don’t fully understand. Maybe the real solution isn’t better timing… but better drugs. Ones that don’t demand such rigid obedience.
Lydia H.
January 27, 2026 AT 19:32My dad took a double dose of his diabetes med last winter. He didn’t say anything until he passed out at the kitchen table. He’s fine now, but… I wish I’d known this. I’m printing this out and taping it to the fridge. Thank you for writing this. You didn’t just give advice-you gave peace of mind.
Malikah Rajap
January 28, 2026 AT 18:21Wait, so if I miss my 8 p.m. dose and remember at 2 a.m., I skip it? But what if I’m still awake? Doesn’t that feel like cheating? Like I’m punishing myself for being human? I get the science… but emotionally, it’s hard. I think we need more compassion in these rules-not just logic.