Penicillin Allergy Assessment Quiz
This tool helps you understand if your past reaction to penicillin was likely a true allergy or just a common side effect. Based on medical research, over 90% of people labeled allergic to penicillin actually aren't. Click "Start Quiz" to begin.
1. When did your reaction happen?
2. What symptoms did you experience?
3. Did you require epinephrine (EpiPen) or medical emergency treatment?
Your Assessment
Most people think they’re allergic to penicillin. But chances are, they’re not.
More than 1 in 10 Americans say they’re allergic to penicillin. That’s over 30 million people. But here’s the shocking part: fewer than 1 in 100 of them actually are. The rest? They’re confusing side effects with true allergies. And that mistake is costing lives, money, and time.
Let’s say you had a rash as a kid after taking penicillin for an ear infection. Your parents told the doctor. The doctor wrote it down. And ever since, you’ve been labeled allergic. You’ve avoided penicillin your whole life. You’ve taken stronger, more expensive antibiotics instead. Maybe you even ended up in the hospital with a C. diff infection because you were given clindamycin instead of a safer, more targeted option. None of that was necessary.
Penicillin is one of the most effective, cheapest, and safest antibiotics ever made. But because so many people think they’re allergic to it, doctors are forced to use alternatives that are less effective, more toxic, and more likely to cause resistance. This isn’t just a personal health issue. It’s a public health crisis.
What’s the difference between an allergy and a side effect?
It’s simple: allergies are your immune system overreacting. Side effects are just your body reacting to the drug-not because it’s attacking it, but because the drug affects things it wasn’t meant to.
True penicillin allergies involve IgE antibodies. These are the same antibodies that cause reactions to bee stings or peanuts. When you’re truly allergic, your body sees penicillin as a threat and triggers a flood of chemicals like histamine. That’s what causes hives, swelling, trouble breathing, or anaphylaxis-life-threatening reactions that happen within minutes to an hour after taking the drug.
But most reactions people call “allergies” aren’t like that. A common rash? That’s often not an allergy. It could be from a virus you had at the same time. Nausea? That’s a side effect. Diarrhea? Common with antibiotics. Vaginal yeast infection? Also common. These aren’t signs your immune system is attacking penicillin. They’re just side effects-unwanted, sometimes annoying, but not dangerous in the way a true allergy is.
And here’s the kicker: if you had a rash more than 10 years ago, you’ve probably outgrown it. Studies show 80% of people lose their penicillin allergy after a decade. Yet most people never get tested.
What does a true penicillin allergy look like?
Immediate reactions (IgE-mediated) are rare but serious. They happen fast:
- Hives (raised, itchy red welts)
- Swelling of the lips, tongue, or throat
- Wheezing or trouble breathing
- Dizziness, rapid pulse, or passing out
- Anaphylaxis (a full-body shock reaction)
If you’ve ever had any of these within an hour of taking penicillin, you need to take it seriously. But even then, you should still get tested. Many people who think they had anaphylaxis actually had a panic attack or a viral illness.
Delayed reactions (non-IgE) are more common and often mislabeled. These show up days later:
- Flat, red rash (maculopapular)
- Fever
- Joint pain
- Swollen lymph nodes
These are rarely true allergies. They’re often caused by viruses like Epstein-Barr or mononucleosis that happen to coincide with antibiotic use. But doctors still write “penicillin allergy” in your chart because they don’t know the difference.
Why does mislabeling matter so much?
It’s not just about avoiding penicillin. It’s about what you get instead.
When you’re labeled allergic, doctors avoid penicillin-even if it’s the best drug for your infection. Instead, they turn to broader-spectrum antibiotics like vancomycin, clindamycin, or fluoroquinolones. These drugs are more expensive. They’re harder on your gut. And they’re far more likely to cause deadly infections like C. diff.
Here’s the data:
- Patients with false penicillin allergy labels are 70% more likely to get a broad-spectrum antibiotic.
- They’re 2.5 times more likely to get C. diff.
- They have 6 more deaths per 1,000 hospitalizations than patients without the label.
- Hospital stays are 0.5 days longer. Costs go up by $463 per admission.
And that’s just the hospital. Outside the hospital, you’re still paying the price. You might get prescribed a more expensive antibiotic that’s less effective. Your infection might linger. You might need more visits. More tests. More drugs.
It’s not just you. It’s everyone. Overuse of broad-spectrum antibiotics fuels antimicrobial resistance. That means more superbugs. Fewer effective drugs. More deaths. This isn’t hypothetical. It’s happening right now.
How do you know if you’re truly allergic?
The answer is simple: get tested. You don’t need to live with a label that’s probably wrong.
There’s a proven three-step process:
- History check - A doctor asks detailed questions about your reaction. When did it happen? What were the symptoms? Did you need epinephrine? Was it a rash or breathing trouble? Tools like PEN-FAST help doctors score your risk.
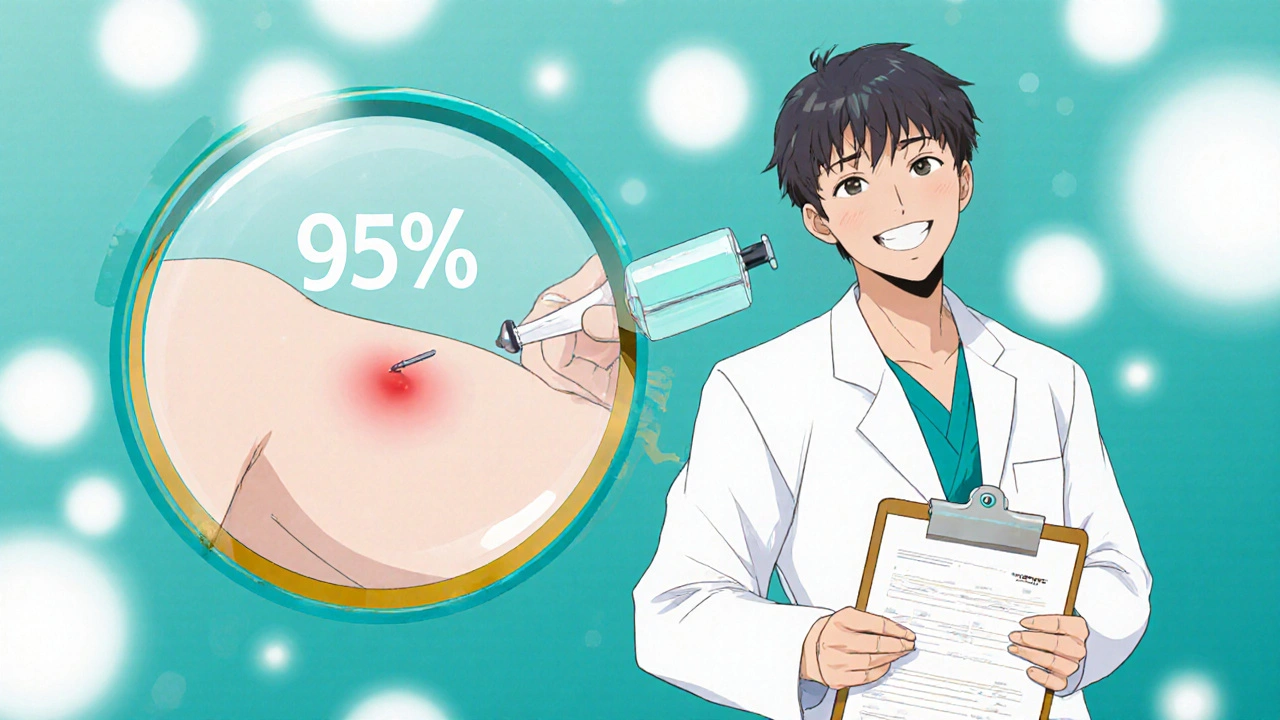
- Skin test - A tiny amount of penicillin is placed under your skin. If you’re allergic, you’ll get a red, itchy bump within 15-20 minutes. This test is 95% accurate.
- Oral challenge - If the skin test is negative, you take a small dose of amoxicillin under supervision. You’re watched for an hour. If nothing happens, you’re not allergic.
This isn’t experimental. It’s standard care. The American Academy of Allergy, Asthma & Immunology says this is the gold standard. Hospitals like Mayo Clinic have done this on over 50,000 patients. Zero deaths. Zero serious reactions during the challenge phase.
And the results? 95% of people who thought they were allergic end up being cleared. They can safely take penicillin again.
What’s stopping people from getting tested?
Three things: fear, access, and ignorance.
Fear: A lot of people are terrified of having a reaction during testing. But here’s the truth: the risk of a serious reaction during testing is lower than the risk of a car ride to the clinic. Most reactions are mild-maybe a little redness or itching. And if something happens, the clinic has epinephrine ready. You’re not alone.
Access: You can’t get tested at your regular doctor’s office. You need an allergist. And not all insurance covers it. Many people don’t even know they need to ask for a referral. A 2021 survey found 45% of patients couldn’t find an allergist covered by their plan.
Ignorance: Even doctors get it wrong. A 2022 study showed only 39% of primary care doctors knew that delayed rashes are rarely true allergies. So they keep writing “penicillin allergy” in charts, even when the history doesn’t fit.
But things are changing. Hospitals are starting pharmacist-led programs. Electronic health records now include prompts to review allergy labels. The CDC has even launched a free smartphone app that helps doctors decide who needs testing.
What should you do if you think you’re allergic?
Don’t assume. Don’t ignore. Don’t wait.
Here’s your action plan:
- Look at your history. Did you have a rash? Was it itchy? Did you break out in hives? Did you have trouble breathing? Did you need an EpiPen? Write it down.
- Ask your doctor. Say: “I think I might have been misdiagnosed. Can you refer me to an allergist for penicillin testing?”
- Be ready to go. The test takes about 90 minutes. You’ll need to clear your schedule. But it’s one of the most important 90 minutes you’ll ever spend.
- Update your records. If you’re cleared, make sure your primary care doctor, pharmacist, and hospital all update your file. Don’t rely on memory.
If you’re over 40 and were labeled allergic as a child? You’re almost certainly not allergic anymore. The antibodies fade. The risk drops. The chance you can safely take penicillin is higher than you think.
The future is changing-fast
In 2025, hospitals will be penalized financially if they don’t fix this problem. Medicare is now tying payments to how well they reduce unnecessary antibiotic use. That means hospitals are investing in testing programs. Pharmacist-led clinics are popping up everywhere. Insurance is starting to cover it better.
Within five years, doctors will routinely ask: “When was your last penicillin reaction?” and then check if you still need the label. It’ll be as normal as checking your blood pressure.
And when that happens, millions of people will finally be able to take the right antibiotic-the one that works best, costs the least, and saves the most lives.
You don’t have to wait. Start today. Ask. Get tested. Take back control of your health.


Clay Johnson
November 30, 2025 AT 05:52The real tragedy isn't the misdiagnosis-it's the institutional inertia that lets it persist. We treat medical labels like permanent tattoos when they're more like temporary ink. The data is clear, the protocols are proven, yet we still let a 10-year-old rash dictate a lifetime of suboptimal care. Why? Because convenience trumps accuracy in healthcare systems built on checkboxes, not critical thinking.
It's not about penicillin. It's about how we assign meaning to symptoms without context. We've outsourced diagnostic responsibility to past records, and now we're paying for it in C. diff rates and antibiotic resistance.
Jermaine Jordan
December 1, 2025 AT 16:54This is one of the most important public health revelations of our generation-and yet, barely anyone knows about it. Imagine if we told people they were allergic to water because they once got sick from a contaminated tap. We wouldn’t let that stand. So why do we let a mislabeled antibiotic reaction define someone’s entire medical identity? The numbers don’t lie: 95% of people labeled allergic aren’t allergic at all. That’s not a glitch. It’s a systemic failure. And it’s costing lives. We need a national campaign. Right now.
Chetan Chauhan
December 2, 2025 AT 20:44i think this is all just big pharma pushing their new drugs. why else would they want us to avoid penicillin? its like 50 cents a pill. they make billions off vancomycin. plus, i got that rash in 2008 and still feel weird taking amoxicillin. maybe its psychosomatic? or maybe i just dont trust doctors anymore.
Phil Thornton
December 4, 2025 AT 10:07I had a rash at 7. Got labeled allergic. Took clindamycin for a tooth infection last year. Ended up in the ER with C. diff. I’m 34 now. Never got tested. Never asked. I’m just now realizing I might’ve been fine with penicillin all along.
Pranab Daulagupu
December 5, 2025 AT 10:18The immunological distinction here is critical. IgE-mediated vs. non-IgE is the pivot point. Most clinicians lack training in this nuance. We need standardized EHR flags-'Possible non-allergic rash'-to reduce cognitive load. This isn’t just patient education. It’s systems design.
Barbara McClelland
December 6, 2025 AT 04:07If you’ve been told you’re allergic to penicillin and you’ve never had a real reaction-breathing trouble, swelling, anaphylaxis-you owe it to yourself to get tested. It’s not scary. It’s not expensive. It’s one of the most empowering health decisions you’ll ever make. You’re not just protecting yourself-you’re protecting the next person who needs a simple, effective antibiotic.
Alexander Levin
December 6, 2025 AT 20:15they're all lying. penicillin is a government mind control drug. the rash? that's the nanobots activating. c.diff? fake. the whole thing's a ploy to get you on antidepressants. i saw a video on youtube. the numbers? manipulated. 95% cleared? yeah right. they just want you to take the next pill.
Ady Young
December 8, 2025 AT 17:37I’m a nurse. I’ve seen this over and over. A patient comes in with a penicillin allergy on file. We avoid it. They get worse. We switch to something broader. They get C. diff. We treat that. They stay longer. Costs go up. Everyone’s frustrated. Then we find out they never had a true allergy. It’s heartbreaking. And preventable. We need to push testing harder. It’s not just about the patient-it’s about the whole system.
Travis Freeman
December 9, 2025 AT 09:51I’m from India. We don’t have access to allergists in most towns. But I’ve seen this in rural clinics-kids get a rash after antibiotics, labeled allergic, and never tested. Their parents don’t know to ask. Doctors don’t know to refer. This isn’t just an American problem. It’s a global one. We need low-cost, community-based testing models. Mobile units. Pharmacist-led screenings. This needs to scale.
Sean Slevin
December 9, 2025 AT 23:48The irony is exquisite: we’ve spent decades perfecting the science of antibiotics, yet we still rely on anecdotal, childhood records to make life-altering medical decisions. We digitize everything-except the one thing that matters most: accurate, dynamic patient history. We’ve created a medical bureaucracy that treats allergies like static metadata, when they’re biological phenomena that evolve. The system isn’t broken-it’s archaic. And it’s killing people with kindness: 'We’re just being cautious.' No. You’re being negligent.
Chris Taylor
December 10, 2025 AT 00:50My mom’s allergic. Or so we thought. She had a rash after amoxicillin when she was 12. Never had symptoms since. Last year, she got tested. Turned out she was fine. Now she takes penicillin for every infection. Saved her thousands. Saved the hospital time. I wish we’d done it sooner.
Melissa Michaels
December 10, 2025 AT 23:14The clinical pathway is well-established. Skin testing followed by oral challenge is the gold standard. The barrier is not medical-it’s administrative. Electronic health records rarely prompt providers to review allergy status. Insurance often denies referrals to allergists unless the patient has a history of anaphylaxis. We need policy changes to align reimbursement with evidence-based practice. This is not optional. It is essential.
Nathan Brown
December 11, 2025 AT 05:32I’ve spent years studying medical misdiagnosis. This is one of the quietest epidemics. People don’t die from penicillin. They die from the antibiotics they’re forced to take instead. The data is irrefutable: 6 more deaths per 1,000 hospitalizations. That’s not a statistic. That’s 6 families shattered every day because we didn’t bother to check if a label was still true. We treat allergies like dog tags-etched in stone. But the body forgets. The system doesn’t. That’s the tragedy.
Matthew Stanford
December 11, 2025 AT 08:27This is the kind of post that makes you feel both hopeful and angry. Hopeful because the solution exists. Angry because it’s so simple and yet so ignored. I’ve talked to my doctor about my childhood rash. She said, 'We’ll refer you.' Then forgot. I had to follow up three times. If this is what it takes for one person, imagine how many never make it through the system. We need a national push-like cancer screenings or flu shots. Penicillin testing should be routine. Not rare.