When you break out in hives after eating peanuts, or your nose won’t stop running every spring, it’s easy to assume you have an allergy. But what exactly are you allergic to? And how do you know for sure? That’s where specific IgE testing comes in. It’s not a magic bullet, but when used right, it can turn guesswork into clear answers.
What Specific IgE Testing Actually Measures
Specific IgE testing looks for antibodies in your blood that react to specific allergens. These are called immunoglobulin E, or IgE, antibodies. When your immune system thinks something like pollen, cat dander, or shellfish is dangerous, it makes these antibodies to fight it off. That’s what triggers your allergy symptoms.
This test doesn’t measure all IgE in your body-that’s total IgE. It zeroes in on IgE tied to one thing at a time: peanut, dust mite, ragweed, egg, etc. Modern labs use a method called Fluorescence Enzyme Immunoassay (FEIA), with ImmunoCAP being the most common platform. It’s precise, reliable, and gives results in kUA/L units. A level below 0.35 kUA/L is considered negative. Anything above that suggests your body has made antibodies to that allergen.
But here’s the catch: finding IgE doesn’t always mean you’ll react when exposed. Some people have detectable IgE but never have symptoms. That’s why results need context. A number alone doesn’t tell the full story.
How It Compares to Skin Testing
For decades, skin prick testing has been the gold standard. A tiny drop of allergen is placed on your skin, then lightly pricked. If you’re allergic, you’ll get a raised bump-like a mosquito bite-within minutes. It’s fast, cheap, and shows real-time biological activity.
But skin testing isn’t always possible. If you have severe eczema covering large areas of skin, or you’re on antihistamines, antidepressants, or other meds that block reactions, skin tests won’t work. That’s where blood tests shine. In fact, about 27% of pediatric patients in the U.S. get blood tests instead because they can’t stop their meds for the 3-5 days needed before skin testing.
Studies show skin tests are slightly more sensitive-about 15-20% better-for common allergens like pollen and dust mites. But modern blood tests have closed that gap. For many allergens, especially foods, the accuracy is now very close. The biggest advantage of blood tests? They’re not affected by medications or skin conditions. And they’re safer if you’ve had a severe reaction before.
What the Numbers Really Mean
Results come as a number: 0.35, 1.2, 5.8, 15.0 kUA/L. Higher numbers usually mean a stronger immune response. But they don’t predict how bad your reaction will be. Someone with a 12 kUA/L peanut result might have a mild rash, while someone with a 4 kUA/L result could go into anaphylaxis.
What matters more is the trend. For peanut allergy, a result of 0.35 kUA/L has only a 50% chance of predicting a true allergy. But at 15 kUA/L, that jumps to 95%. That’s why doctors don’t just look at one number-they look at the pattern, your history, and what’s happened in the past.
Weak positives (0.35-0.70 kUA/L) are tricky. They could mean a real allergy, or they could just be noise. That’s why labs now automatically check your total IgE level when a specific IgE comes back positive. If your total IgE is sky-high (say, 100 kUA/L), then a 0.5 kUA/L peanut result is tiny-only 0.5% of your total antibodies. But if your total IgE is only 1 kUA/L, then 0.5 kUA/L is half of it. That changes everything.
When You Should-and Shouldn’t-Get Tested
Testing makes sense when your symptoms clearly point to an IgE-mediated allergy: hives within minutes of eating, wheezing after being around cats, swelling after a bee sting. It’s also used to confirm allergies before starting immunotherapy.
But too many people get tested for the wrong reasons. The National Guideline for Laboratory Testing (2025) found that 22% of tests ordered in primary care are unnecessary. Why? Because doctors test for everything-every food, every pollen-just because they can.
That’s dangerous. Testing too many things at once increases false positives. If you test for 20 allergens, pure chance says you’ll get 1-2 positive results even if you’re not allergic. That leads to unnecessary food avoidance, anxiety, and even malnutrition.
Guidelines say: test only what makes sense based on your history. If you’ve eaten peanuts for 30 years without issue, don’t test for them. If you’ve never been near a cat and have no symptoms, skip cat dander. And never order a “food panel” with 10+ items. The same guideline bans food mix tests because they’re wrong more than 30% of the time.
What’s New in Allergy Testing
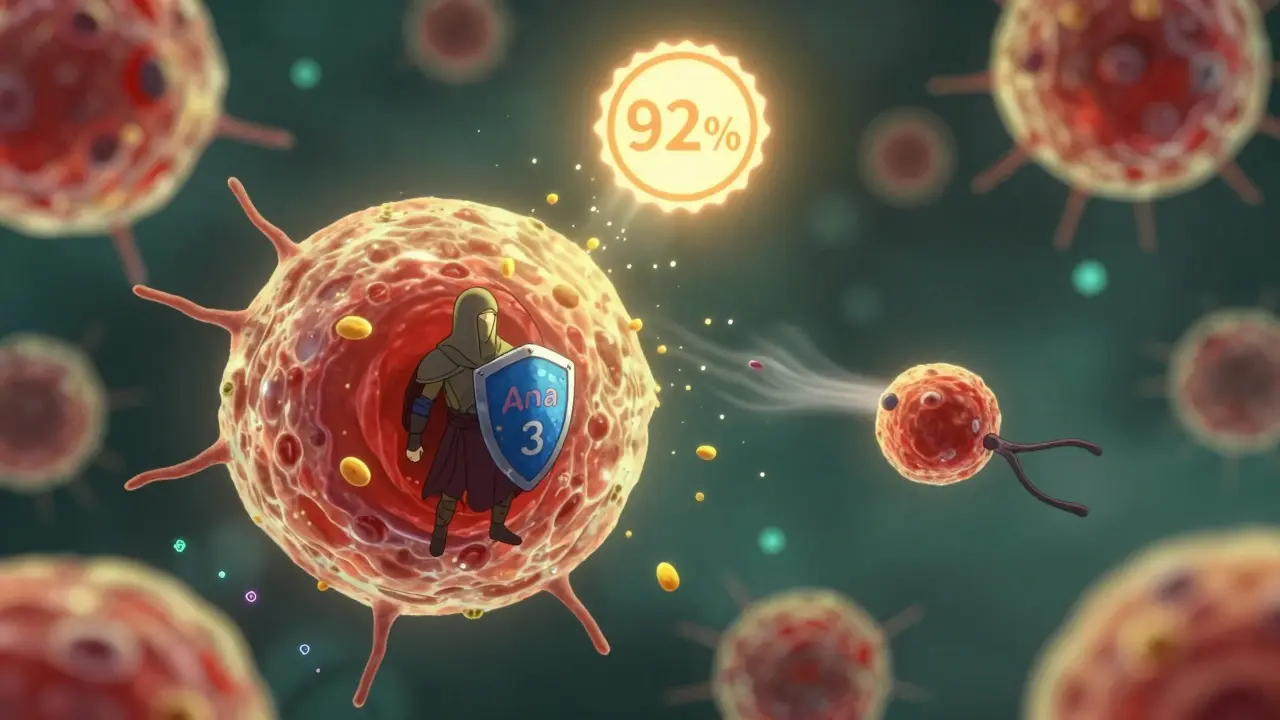
Recent advances are making testing smarter. Component-resolved diagnostics (CRD) look at individual proteins within an allergen, not just the whole thing. For example, cashew nut has several proteins. One protein (Ana o 3) is linked to severe reactions. Another (Profilin) causes mild symptoms and often cross-reacts with birch pollen. CRD can tell the difference.
Old methods had 70% accuracy for nut allergies. CRD bumps that to 92%. That’s huge. It means fewer people avoid nuts they’re not truly allergic to.
Another innovation is the ImmunoSolid Phase Allergen Chip (ISAC), which tests for 112 allergen components from just 20 microliters of blood. Sounds impressive, right? But it’s not for everyone. Interpretation is complex. Only specialized allergy centers should use it. Most clinics still stick to single allergen tests because they’re simpler and just as effective when used properly.
How to Get the Most Out of Your Test
Don’t walk into a lab and ask for a full panel. Talk to your doctor first. Ask: What symptoms am I having? When do they happen? What triggers them? If you get a positive result, ask: What does this number mean for me? Is this a true allergy or just sensitization?
Also, don’t retest unless something changes. If you were told you’re allergic to eggs at age 2 and haven’t had a reaction since, retesting isn’t needed unless you’re considering reintroducing them. Retesting people with known tolerance adds no value-and 38% of inappropriate testing happens exactly because of this.
And remember: results take 3-5 days. This isn’t an emergency test. It’s for planning, not crisis management.
What Happens After the Test?
If the test confirms an allergy, your doctor will help you build a plan. That might mean avoiding the allergen, carrying an epinephrine auto-injector, or starting immunotherapy. For food allergies, you might work with a dietitian to ensure you’re still getting proper nutrition.
If the test is negative but symptoms persist, it’s time to look elsewhere. Not all reactions are IgE-mediated. Some are caused by food intolerances, chemical sensitivities, or even stress. A negative IgE test doesn’t mean nothing’s wrong-it just means it’s not an IgE allergy.
And if you’re unsure about your results? Seek a specialist. Allergists are trained to interpret these numbers in context. A general practitioner might see a 1.2 kUA/L result and say, “You’re allergic.” An allergist will ask: “What happened when you ate it last? Have you ever had a reaction? What’s your total IgE?”
Specific IgE testing is a powerful tool. But like any tool, it’s only as good as the person using it. Used wisely, it can free you from fear. Used carelessly, it can lock you into a life of unnecessary restrictions. Know your numbers. Understand your history. And never let a lab result override your own experience.
Is specific IgE testing the same as a food allergy test?
Yes, but it’s more precise. A "food allergy test" is often a vague term. Specific IgE testing measures IgE antibodies to individual foods like peanut, milk, or shellfish. It’s not a general screen-it’s targeted. Avoid broad "food panels"-they’re unreliable. Stick to testing only what your symptoms suggest.
Can I get a false positive on a specific IgE test?
Absolutely. A positive result means your body made antibodies, but not that you’ll react when exposed. About 50% of people with low-level IgE (0.35-0.70 kUA/L) never have symptoms. This is called sensitization, not allergy. That’s why your clinical history matters more than the number.
How long does it take to get results?
Most labs deliver results in 3 business days. Some rare allergens require sending samples to specialized centers, which can take up to 7-10 days. This isn’t an urgent test-it’s for planning, not emergencies. Don’t expect same-day results.
Do I need to stop my medications before the test?
No. Unlike skin testing, blood tests aren’t affected by antihistamines, asthma meds, or antidepressants. You can take your regular medications. That’s one of the biggest advantages of IgE testing-no prep needed.
Can specific IgE testing predict how bad my reaction will be?
Not reliably. Higher IgE levels (like 15 kUA/L for peanut) suggest a higher chance of a reaction, but they don’t predict severity. Someone with a low number can have a life-threatening reaction. Only your past history and a doctor’s evaluation can help estimate risk.
Is component-resolved diagnostics worth it?
It can be, but only if you’re seeing an allergist. CRD looks at individual proteins in an allergen-like distinguishing a dangerous cashew protein from a harmless one that cross-reacts with birch pollen. It improves accuracy from 70% to 92%. But it’s complex, expensive, and not needed for most people. Ask your allergist if it applies to your case.
Should I get tested for allergies if I’ve never had symptoms?
No. Testing people without symptoms leads to false positives and unnecessary fear. If you’ve eaten peanuts, shellfish, or dairy your whole life without issue, don’t test for them. Allergy testing is for diagnosing existing problems-not screening healthy people.


Molly Silvernale
January 9, 2026 AT 01:04So it’s not about the number-it’s about the story behind it? That’s wild. I used to think a high IgE level meant doom, but now I realize it’s just a whisper from my immune system, not a scream. It’s like seeing a red light on a dashboard-doesn’t mean the engine’s blown, just that something’s lit up. And if you’ve never had a reaction? Maybe it’s just your body being overly polite to pollen.
Also, why do we treat antibodies like destiny? We’re not machines. We’re messy, adaptive, evolving organisms. That 0.5 kUA/L result? Could be noise. Could be a ghost. Could be your body practicing for a threat that never comes. Let’s stop pathologizing sensitivity.
Ken Porter
January 10, 2026 AT 23:01Testing everyone for everything is a joke. American medicine is broken. You don’t need a blood test to know you’re allergic to shellfish if you’ve thrown up after eating it since you were five. Stop letting labs make money off fear. I’ve seen people avoid dairy because of a 0.4 result and then get calcium deficiency. That’s not science-that’s corporate greed wrapped in a white coat.
Manish Kumar
January 12, 2026 AT 17:02Look, I’ve been thinking about this for days now, and it’s actually a metaphysical question disguised as immunology. We’re measuring antibodies, sure, but what are we really measuring? The body’s fear response? The mind’s imprint on biology? The immune system doesn’t know what peanut is-it just knows something triggered it once, and now it’s stuck in a loop. Is that allergy? Or is that trauma encoded in protein form? And if CRD can distinguish between dangerous and harmless proteins, doesn’t that suggest our bodies are more nuanced than our labels? We call it peanut allergy, but maybe it’s just a miscommunication between molecules and memory. We’re so quick to name things, but the truth is far stranger. The body doesn’t lie-but our interpretations? Oh, they lie all the time.
Donny Airlangga
January 12, 2026 AT 17:11This is the most balanced, thoughtful piece on IgE testing I’ve ever read. I’ve had two anaphylactic reactions to cashew, and my IgE was 22. But I also know people with 18 who never reacted. It’s not the number. It’s the history. My allergist didn’t just look at the lab sheet-he asked me what happened the first time I ate cashew, what my mom said, how scared I was. That’s the real diagnostic tool. Thank you for saying this out loud.
Lois Li
January 14, 2026 AT 14:35I’m so glad someone wrote this. I used to get tested for every food under the sun because my mom was paranoid. Got 7 positives. Avoided 7 foods. Lost 15 pounds. Got anxiety. Turned 25, went to an allergist, and they said ‘You’ve eaten all of these your whole life without issue-why are you scared?’ Turned out four of those were false positives. Total IgE was sky high from eczema. My body was just screaming for help, and the test misinterpreted it as ‘allergy.’ I’m eating peanut butter again. I’m alive. And I’m not sorry.
christy lianto
January 15, 2026 AT 07:16CRD is a game-changer. I had a kid with a 1.2 kUA/L peanut result. We did CRD-turns out it was profilin, not Ara h 2. He can eat roasted peanuts now. No reaction. No fear. No anxiety. No missed birthday cakes. This isn’t just science-it’s freedom. Why are we still using 1990s logic when we have 2025 tools? Stop testing everything. Start testing smart. Your life depends on it.
swati Thounaojam
January 16, 2026 AT 04:31My sister got tested for 15 foods after a rash. 3 positives. Avoided all. Got sick. Lost weight. Turns out she had celiac. IgE test was useless. Don’t trust numbers without context. Always ask: what’s really going on?
Annette Robinson
January 16, 2026 AT 12:36This is the kind of post that changes lives. Thank you for writing it with such clarity. To anyone reading this: if you’ve ever been told you’re allergic because of a lab result alone, please-find an allergist. Don’t let a number define your diet, your joy, your freedom. Your history matters more than your blood. And if you’re a clinician? Please, test only what makes sense. You’re not just ordering a test-you’re shaping someone’s life.