Diabetes Meds: What Works, What to Watch For, and How to Stay on Track
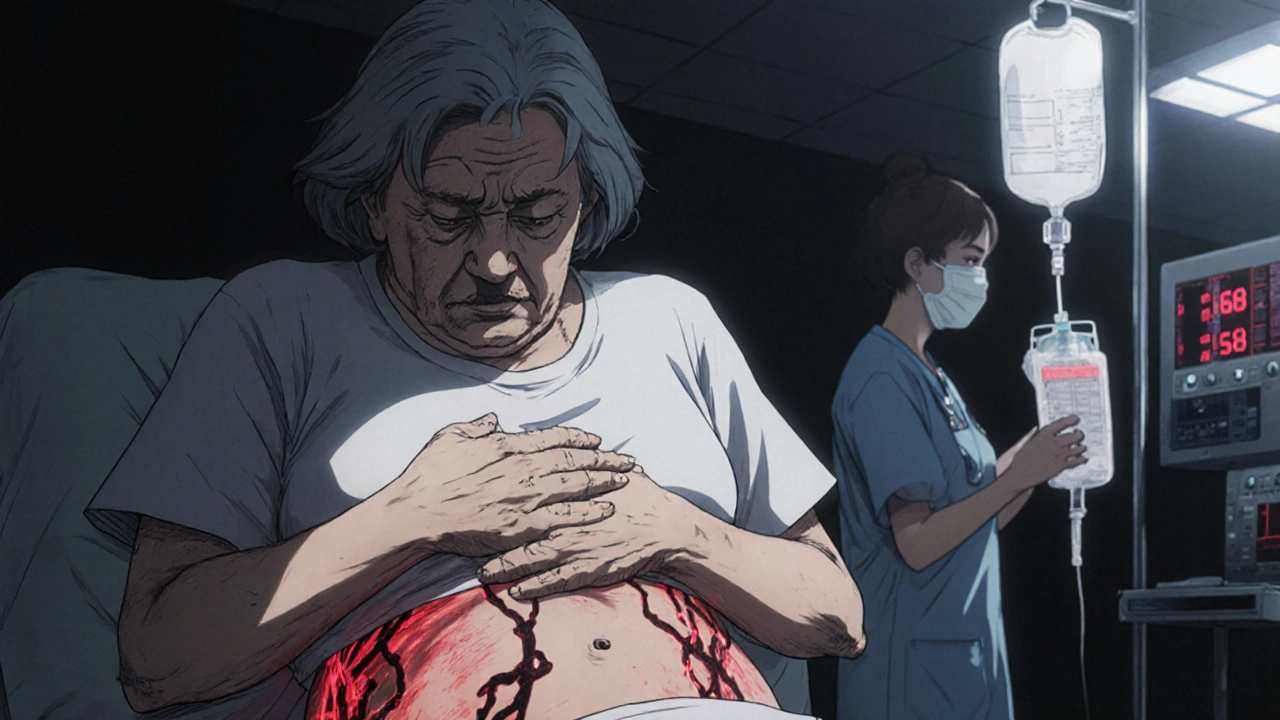
When you have diabetes, a condition where the body can’t properly use or make insulin to control blood sugar. Also known as hyperglycemia, it’s not just about sugar—it’s about how your body handles energy. Without the right diabetes meds, prescription drugs designed to lower or manage blood glucose levels, your risk for nerve damage, kidney failure, and heart problems goes up fast.
Not all diabetes meds are the same. Some, like metformin, the most common first-line drug for type 2 diabetes that reduces liver sugar production and improves insulin sensitivity, are taken daily and rarely cause low blood sugar. Others, like insulin, a hormone injected to replace what the body doesn’t make, used in both type 1 and advanced type 2 diabetes, need careful timing and dose tracking. Then there are newer options like SGLT2 inhibitors and GLP-1 agonists that help with weight loss and heart protection—but they come with their own side effects, like yeast infections or nausea. Many people stop taking their meds because of these side effects, not because they don’t work. In fact, medication adherence, how consistently someone takes their prescribed drugs, is the biggest barrier to good control, not cost or forgetfulness.
What you take depends on your type of diabetes, your weight, your other health issues, and even your daily routine. Some people need just one pill. Others juggle multiple drugs, injections, and constant monitoring. The goal isn’t just to hit a number on a glucose meter—it’s to live without the crashes, the fatigue, and the long-term damage. The posts below cover real-world stories and science: how metformin affects your gut, why insulin dosing can be tricky in seniors, what to do when a drug stops working, and how side effects like nausea or dizziness make people quit—even when they know they need it. You’ll find clear advice on switching meds, spotting warning signs, and staying on track without feeling overwhelmed.