SGLT-2 Inhibitors: How They Work, Who They Help, and What You Need to Know
When you hear SGLT-2 inhibitors, a class of oral diabetes medications that lower blood sugar by making the kidneys remove glucose through urine. Also known as gliflozins, these drugs don’t just control sugar—they change how your body handles energy, fluid, and even heart stress. Unlike older diabetes pills that push your pancreas to make more insulin, SGLT-2 inhibitors work downstream, letting your kidneys do the heavy lifting. That’s why they’re often used when insulin isn’t enough—or when you need protection beyond blood sugar control.
These drugs are closely tied to three key names you’ll see on prescriptions: empagliflozin, a SGLT-2 inhibitor proven to reduce heart failure hospitalizations in people with type 2 diabetes and heart disease, dapagliflozin, one of the first approved and now used for heart failure even without diabetes, and canagliflozin, known for its strong effect on kidney protection in high-risk patients. Each has subtle differences in how they’re dosed or what side effects they carry, but they all share the same core mechanism: blocking a protein in your kidneys called SGLT-2 that normally reabsorbs glucose back into your blood. By stopping that, you flush out 60 to 90 grams of sugar a day—roughly 240 to 360 calories worth.
That’s not just a blood sugar trick. This daily sugar loss also pulls water with it, lowering blood pressure and reducing swelling. It’s why these drugs are now first-line for people with heart failure or chronic kidney disease—even if they don’t have diabetes. Studies show they cut the risk of hospital stays for heart failure by up to 30% and slow kidney decline in people with protein in their urine. They’re not magic, but they’re one of the few diabetes drugs with real proof of saving lives, not just numbers.
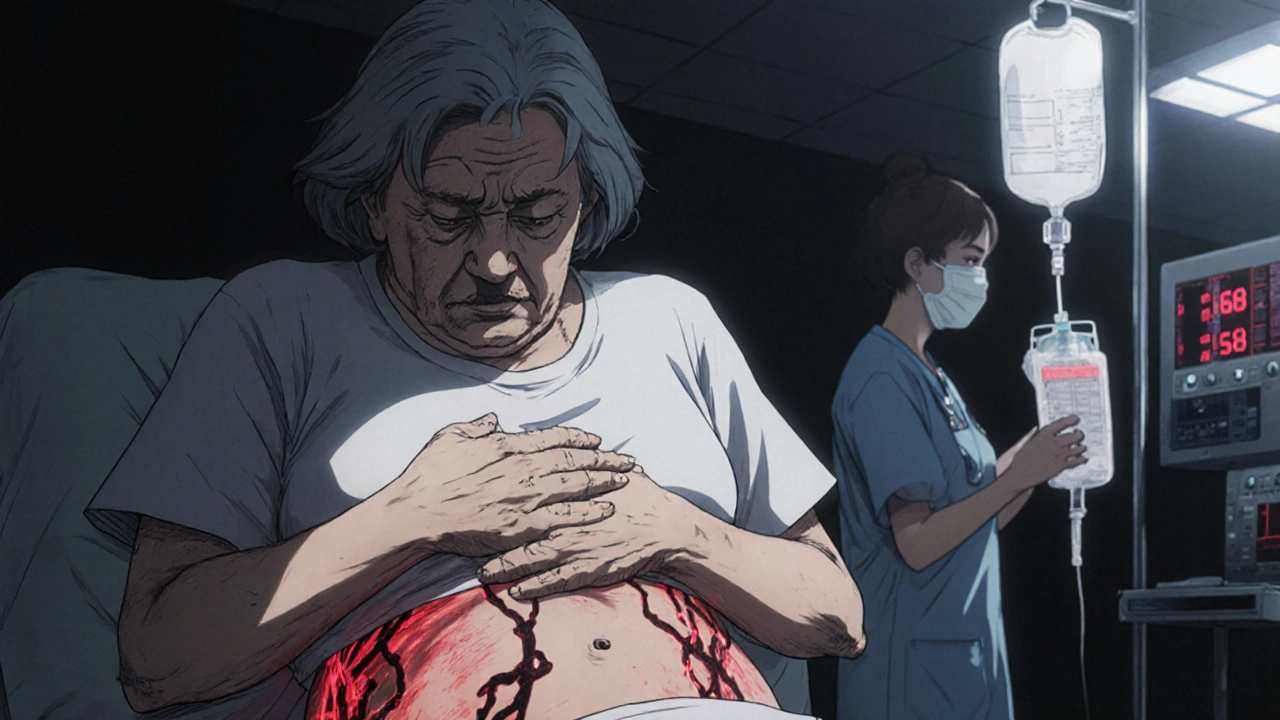
But they’re not without trade-offs. More frequent yeast infections, especially in women, and a small risk of rare but serious genital infections are common. Dehydration and low blood pressure can happen, especially if you’re also on diuretics. And while they don’t cause low blood sugar on their own, combining them with insulin or sulfonylureas can. That’s why you need to talk to your doctor before starting—not just about sugar, but about your fluid intake, kidney function, and whether you’re at risk for DKA, a rare but dangerous condition even when blood sugar looks normal.
What you’ll find below are real-world stories and science-backed guides about how these drugs fit into daily life. From how they interact with other meds like metformin or insulin, to what to do when side effects pop up, to how they compare with newer options like GLP-1 agonists. You’ll see how people manage the bathroom frequency, why some stop taking them, and how doctors decide who benefits most. These aren’t theoretical discussions—they’re from patients and providers who’ve lived with these drugs, adjusted doses, dealt with side effects, and found what works.